People often suffer from ridicule from others about their height. At the genetic level, as a result of injuries, hormonal imbalances or other reasons, a person can be significantly shorter than his peers. This is especially fraught for the stronger half of humanity, who, due to their short stature, suffer from a lack of female attention.
As for the fair half of humanity, they also do not breathe evenly to the length of their legs. It is known that many girls would like to become models, where tall height is a necessary part of the requirements for any candidate. And in everyday life, men are attracted to long-legged, slender girls. Indispensable heels come to the aid of short stature, but you don’t always want to wear them, and they’re not entirely safe. In such cases, there are two options - lengthening the legs through surgery or a set of exercises.
Let's grow before it's too late
The safest method of growing taller without surgery is to stimulate natural growth. Up to a certain age, when growth zones are still open, a person, using special exercises, can add a few centimeters.
It is best to do the developed complex in the morning and evening. After waking up, the human spine is in a relaxed-elongated state, so the exercises will be aimed at stretching the torso by additional centimeters. Exercising in the evening, when the spine has “formed”, will help consolidate the results achieved in the morning and improve the health of the body.
The lengthening of the legs itself occurs due to the build-up of cartilage in the knee joint as a result of its stretching and enlargement. The effectiveness of the exercises will increase if you do them at least three times a week, for at least 15 minutes a day.
With regular training, the pituitary gland is stimulated, which promotes the production of growth hormone, which has a positive effect on the final results. So, in six months you can grow by 5-10 sentiments.
The list of the most accessible and effective exercises includes:
- Lengthening your legs with inversion boots. The essence of the exercise is to stretch the knee, hip joints and bones under the influence of gravity. Boots must be put on the ankles and, having climbed the horizontal bar, hang head down for no more than half an hour. To begin with, being in an inverted position for 3 minutes is enough. Then the time should be increased depending on the body’s tolerance to the inverted state.
- The growth of cartilage tissue between the tibia and femur is also carried out using weights. The duration of the exercise is from 15 to 30 minutes. You need to sit on a high chair or any other elevation that seems comfortable but firm. In this case, your feet should not touch the floor. For the first few sessions, weights with a relatively small weight are put on the ankles (every few approaches the weight must be increased). The training system on a chair is as follows: we stretch for 5-10 minutes, do light swings with our legs forward for 5-10 minutes, and do more intense swings for 5-10 minutes.
Results guaranteed
No one can guarantee that everything will work out the way you planned:
That is, it may well not be possible to grow by the promised 10 cm due to poor tissue extensibility or premature closure of growth zones.
- Theoretically, growth zones are open until 16 years of age, but this is a relative indicator: some people finish growing earlier, some later.
- In adolescence, the operation will achieve the best effect; in more mature age, the result can be much worse.
- The whole paradox and injustice is that the possibilities of lengthening are directly proportional to your height - this means: the taller the girl, the more cm she can lengthen her legs;
- on the contrary, a naturally small girl is unlikely to be able to easily increase 7–10 cm.
Bottom line: is it worth the risk and suffering for perhaps two unfortunate added centimeters?
If it's too late to grow...
…it’s time to contact specialists at the center of orthopedic cosmetology and correction. Leg lengthening through surgery is carried out using the Ilizirov apparatus. The process lasts on average for six months. This will be followed by several months of rehabilitation.
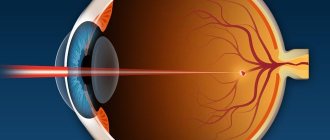
The operation to increase height takes place in several stages and consists of performing a surgical fracture of the tibia and fibula in the tibia or femur:
- Osteomatia - during the operation under general anesthesia, several incisions are made on the leg through which the surgeon dissects the bone. Then the Ilizirov apparatus wires are inserted into them, which fix the bone fragments. The brace will need to be worn throughout the heightening process. In some clinics, both legs are lengthened at once, in others - alternately with an interval of 1 month.
- Distraction is the lengthening of the limbs by the patient, which begins 3-7 days after osteomaty surgery. It consists of daily lengthening of the legs by 0.75-1 millimeter. The patient manually tightens the nuts of the device about 4 times a day. On average, in 50 days you can grow at least 5 centimeters.
- Fixation is a period of rehabilitation. Lasts twice as long as the previous stage. Aimed at strengthening young bone areas.
During 3 stages, the patient must be under the supervision of doctors and move with the help of crutches. In rare cases, it is allowed to undergo the leg lengthening process on an outpatient basis. During the entire time spent in the Illizirov apparatus, the patient must daily disinfect the incisions into which the needles are inserted. Failure to comply with this instruction may result in the device being removed prematurely due to the development of infection.
After the fixation period, sports activities are allowed after 2-3 months. In the first 1-2 months after rehabilitation, it is recommended to go swimming and do moderate walking.
Preparation for the procedure
Before scheduling the day of surgery, the patient must meet with the doctor several times. At the first visit, the skeletal system is examined and general tests are taken in order to exclude serious concomitant diseases that may serve as a contraindication to surgery.
Afterwards, the patient receives individual recommendations for preparation. From this moment until the implants are implanted, several months pass. 1.5 months before the intervention, the patient again visits the clinic, where some repeated studies are carried out, and the quality of the patient’s preparation is assessed.
Prices for leg lengthening in Germany are determined by many individual factors, the main one of which is the desired result. After a conversation with a specialist, a preliminary cost calculated for a specific patient will be given.
It should be noted that leg lengthening is a long process that is very difficult to complete on your own. Therefore, our team offers you a helping hand. We will not only select an experienced specialist with knowledge of the matter for you, but will also ensure communication with the doctor throughout the entire therapy. We will regularly arrange for you to communicate with a doctor, where a specialist will be able to note the success achieved during therapy, review the results of examinations and answer all your questions. With us, leg lengthening abroad will take place for you without any problems or unforeseen situations.
The importance of choice
Before deciding on the need to increase height through surgery, you should weigh all the PROs and CONS by reading the photos before and after surgery, the consequences and possible dangers:
- Infection. If you skip at least one treatment of wounds with antiseptic solutions, you can catch a serious infection, which will lead to osteomyelitis. As a result, you may need to take antibiotics and additional surgery to remove or replace the wires. In the worst case, the process of lengthening the legs may be suspended until the infection is eliminated.
- Prolonged pain. During the operation, a surgical fracture is made, which feels like a real one. Pain may be present for most of the lengthening, if not the entire period.
- Risk of device breakdown. This will require additional surgical intervention to replace it.
- Bleeding during needle insertion. It is fraught with the formation of a hematoma, which can be eliminated during an additional operation.
Osteosynthesis and osteotomy
All lengthening operations are based on osteosynthesis - the properties of bone cells to divide.
Attention: Osteosynthesis is preceded by an osteotomy - an intersection (fracture) of a bone, that is, before adding a couple of centimeters to your legs, they will first be drilled out with a drill, and then, roughly speaking, they will simply be broken.
For the impressionable, of course, it’s better not to see this.
The operation is performed using the method of osteotomy - leg fracture
And then the osteosynthesis itself will begin - the long process of bone healing (after a fracture) with all the accompanying:
- scarring, adhesions, incomplete fusion;
- muscle contractures;
- postoperative pain;
- long-lasting wounds on the skin, etc.
To find out what people typically experience during this time, talk to those who have had tragic experiences with trauma.
Healing during limb lengthening is burdened by the need for daily distraction, and therefore takes much longer than with a normal fracture
It's not all bad
Israeli medicine has introduced innovation into the Ilizirov leg lengthening method. Instead of a bulky device, experts have developed special pins that are inserted into the bone and secured with bolts. After this, the doctor makes a surgical fracture and after some time, using a remote control, gradually moves the pins apart, increasing the length of the rod inserted with them.
Reviews and results from those who have tested the innovation indicate that the developed method is more gentle, safer, but also more expensive. Using pins, the legs can be lengthened by 6.5 centimeters.
How is leg lengthening surgery performed?
If girls knew about the procedure of the operation itself, about all the side effects and complications after it, about how long this whole painful process lasts, then there would be much less people willing to lengthen their legs.
In orthopedics, operations on the limbs are extremely important and are performed in the following cases:
- For complex open fractures of the tibia.
- To correct severe V-shaped or C-shaped curvature of the limbs.
- Elimination of the defect of difference in leg length.
- For joint replacement.
In any of these cases, there are medical indications for surgery:
- motor dysfunction,
- severe pain,
- pronounced lameness,
- influence on the biomechanics of the spine, etc.
A little about cosmetic orthopedics
Cosmetic orthopedics is a branch of surgery that deals with surgical intervention in the structure of the musculoskeletal system of a patient who wants to change the parameters of the limbs. As a rule, there are no special indications for such leg lengthening operations.
Today there are the following types of orthopedic operations:
- Changes in the shape, length and width of the foot.
- Elimination of curvature of legs.
- Lengthening the femur or tibia.
Often specialists see no particular reason to resort to such an operation. While the patient himself sees the following shortcomings in himself:
- Crooked legs. Often people who have this defect not too pronounced turn to surgery for help. However, many consider surgery to be the only solution.
- Large foot size. Today, manufacturers take into account the parameters of the legs of the current “Cinderellas” and sew from 36 to 41. However, this does not stop some beauties who want to be a few centimeters taller.
- Model parameters today force many girls to change their appearance: enlarge their lips, correct the shape of their nose, as well as the length of their legs. However, in this case, tall height and small foot size are incompatible, then the young ladies have certain problems with the proportions in the body, and, accordingly, health.
Treatment of leg length discrepancy in children in Israel – prices
Compared to European and American, Canadian and Asian clinics, treatment in Israeli hospitals allows you to save up to 25-45% of money. Affordable prices for correction of lower extremity asymmetry attract patients from all over the world to our clinic.
You can find out prices now from our managers by phone or online. It should be borne in mind that the prices announced by the consultant are prices for diagnostic and treatment procedures. You can calculate the cost of your treatment only after drawing up your program.
Advantages of correcting leg length discrepancies in children at the Ichilov Complex center
High-quality treatment of leg length discrepancies in children in Israel is receiving positive reviews, and in increasing numbers every year. In the vast majority of cases, our doctors manage to correct leg asymmetry, regardless of its severity. The skill and experience of orthopedists at the Ikhilov Complex center allows us to correct discrepancies in the length of the lower limbs in children up to 10-20 cm.
- The clinic employs specialists whose experience and qualifications would be the envy of any European or American clinic. Many of our doctors participate in scientific research and are involved in the development of global orthopedics.
- The Ichilov Complex Center is equipped with modern diagnostic equipment that allows you to differentiate leg length discrepancies from other injuries and deformities of the limbs, and clearly monitor progress in treatment.
- In the person of a curator-translator, you receive a personal assistant who helps in solving various issues (transfer, accommodation, translation of documents, etc.) and coordinates interaction with medical staff.
- 5
- 4
- 3
- 2
- 1
(6 votes, average: 4.5 out of 5)
Side effects and possible complications
- While the device is on your feet, you will have to take a lot of painkillers, and they hit many organs, especially the stomach and intestines.
- The needles of the Ilizarov apparatus often burst when walking and have to be changed frequently, and this is also an operation with local anesthesia.
- Because of the knitting needles, the skin on the legs is constantly injured, stitches and wounds on the skin of the legs cause a lot of inconvenience: pain, itching and irritation, plus they are aesthetically unsightly. (But this is all fixable, since sooner or later the device will be removed and everything will heal).
- If after the operation there are too rough scars and scars from the needles, the surgeon can subsequently correct them using light plastic surgery.
- To improve results (especially with closed growth areas), surgery is usually accompanied by the prescription of growth hormones, and this can lead to weight loss or some other troubles that hormones often bring, disrupting the natural hormonal balance.
- Wearing the device on the lower leg for a long time leads to incomplete flexion and extension of the leg and the formation of contracture.
- Correction of contractures is possible only through enhanced rehabilitation, otherwise lengthening may ultimately result in lameness, muscle atrophy, and asymmetry.
- Frequent complications after surgery using the Ilizarov apparatus are arthrosis of the foot, ankle and knee joints.
Adapted technique for lengthening tubular bones using a combined method
Dzhumabekov S.A., Kuluev T.M. Bishkek Research Center for Traumatology and Orthopedics, Bishkek.
Abstract: A combined method of lengthening large tubular bones of the lower limb, adapted to real clinical conditions with minimal technical equipment. Description of the technique, research results, conclusions.
Key words: lengthening of tubular bones, combined method of bone lengthening.
Abstract: Combined method of lengthening the large tubular bones of the lower limbs adapted to the real conditions of the clinic with minimal technical equipment. Description of technology and research findings, conclusions
Keywords: lengthening of long bones, combined bone lengthening method.
Introduction: In terms of limb lengthening technologies, there has currently been significant progress, but it still remains labor-intensive, difficult to perform, time-consuming in relation to the final result, and most importantly, prone to numerous complications. However, the number of patients with deforming shortenings of the lower extremities is increasing every year. Thus, according to some domestic and foreign authors, the number of patients requiring lengthening of one or two limb segments out of all orthopedic and traumatological patients can reach up to 50% [G.A. Ilizarov, 1984; A.I. Bliskunov, 1983; S.A. Dzhumabekov, 1990; IN AND. Shevtsov, 2003; Artemyev A.A., 2008; Aranovich A.M., 2011; Guichet JM, 2003; Abbaspour A., 2008; Klimov O.V., 2010].
Along with orthopedic patients, in recent years the number of requests from somatically healthy people to increase their height has increased. [Bliskunov A.I., 1983; Dzhumabekov S.A., 1990; Sokolovsky O.A., 2000; Tsunakov V.E., 2007; Vvedensky S.P., 2010; Tushina N.V., 2012; Kocaoglu M., 2004].
Currently, there are two main directions in limb lengthening: the method of lengthening with extrafocal osteosynthesis devices (Charnley, Hoffmann, Roger-Anderson, AO-ASIF, Fischer, Hoffmann-Vidal, Gudushauri, Sivasha, Volkova-Oganesyan, Ilizarov, Kalnberza, Ettinger, Taylor Spatial Frame, BIOMET Hybrid External Fixator, Ortofix Hybrid External Fixator) and submersible intramedullary distractors (Bliskunova, Dragana, Ortofix, Precise Nadel, Fitbone). In the countries of the former CIS, the devices of A.I. Bliskunov are most widely used. and Ilizarova G.A.
Suggested by G.A. Ilizarov’s method of transosseous compression-distraction osteosynthesis made it possible to comprehensively solve the problem of limb lengthening and elimination of associated deformities. Optimization of the conditions for regeneration and functional restoration of the lengthened segment was achieved due to the low traumatic nature of the surgical intervention, preservation of the blood supply to the fragments, individually selected pace and rhythm of their traction, as well as the possibility of early functional load on the limb. The consequence of this was a significant reduction in treatment time, its morbidity, and the number of postoperative complications. However, when using this method, there are a number of negative factors: a long stay of the limb in the apparatus until complete ossification of the bone regenerate, uncomfortable conditions for the patient due to the presence of a bulky apparatus in the area of the limb being lengthened, unstable fixation of fragments and bone regenerate, the possibility of secondary mixing of fragments (stability achieved by increasing the fixation elements). High risk of wire osteomyelitis due to prolonged placement of Kirschner wires in the area of the limb being lengthened. Development of myogenic contractures of the knee joint due to the presence of the apparatus and knitting needles in the thigh area (stitching of muscles and integumentary tissues with knitting needles) [G.A. Ilizarov, 1984; V.I.Shevtsov, 2003].
The Bliskunov technique differs favorably from the Ilizarov technique in that the distractor is located intramedullary, the patient feels comfortable during the treatment period, the risk of infectious complications is minimized by the interstitial location of the distractor (there is no communication with the environment), and there are no conditions for mixing fragments due to rigid fixation. Despite all the advantages of this technique, there are indirect disadvantages, which include: high-tech expensive instruments, inaccessibility for a wide range of orthopedic traumatologists due to the complexity of surgical manipulations [Bliskunov A.I., 1983; Dzhumabekov S.A., 1990; Shevtsov V.I., 2003; Aranovich A.M., 2011; Guichet JM, 2003; Birch JG, 2004]. All this indirectly relates to the situation in our Republic. The lack of high-tech instrumentation, the high cost of implants for lengthening, and the inaccessibility of modern technologies to local specialists leads to disastrous results of attempted lengthening, and many patients, due to lack of information, sometimes do not know that this is possible.
Considering these circumstances, there is an urgent need to develop a technique for lengthening large tubular bones adapted to the realities of the clinic.
Materials and methods: Patients examined as part of our scientific work were hospitalized in the departments of joint pathology and pediatric orthopedics of the Bishkek Research Center for Traumatology and Orthopedics for the period from 2007 to 2014. To state a scientific fact on a clear evidence base, all patients with acquired or congenital shortening of the lower limb were divided into two groups: the main group - 49 (47.1%) patients and the control group - 55 (52.9%) patients, which ultimately amounted to 104 patients. In both groups, for comparative assessment, equal proportions were observed in terms of age, clinical and radiological manifestations of the disease. The only difference is the treatment method used: in the main group, the new developments we proposed were used, and in the control group, treatment was carried out according to the standard regimen.
The most common reasons that prompted patients to seek highly qualified orthopedic care at the outpatient diagnostic department of the Bishkek Research Center for Traumatology and Orthopedics were the following diseases, which are shown in Table 1.
Table 1 – Distribution of patients by nosology
| Nosology | Main group | Control group | Total | |||
| abs.h | % | abs.h. | % | abs.h. | % | |
| Post-traumatic shortenings | 12 | 24.5 | 12 | 21.8 | 24 | 23.1 |
| Consequences of osteomyelitis | 3 | 6.1 | 9 | 16.4 | 12 | 11.5 |
| Consequences of polymyelitis | 6 | 12.2 | 6 | 10.9 | 12 | 11.5 |
| Congenital hip dislocation | 12 | 24.5 | 12 | 21.8 | 24 | 23.1 |
| Hip dysplasia | 7 | 14.3 | 6 | 10.9 | 13 | 12.5 |
| Pathological hip dislocation | 5 | 10.2 | 5 | 9.1 | 10 | 9.6 |
| Congenital shortenings | 4 | 8.2 | 5 | 9.1 | 9 | 8.7 |
| Total | 49 | 100,0 | 55 | 100,0 | 104 | 100,0 |
| Representativeness error M±σ | 7±3.65 | 7.8±3.1 | 14.8±6.38 | |||
In addition, we identified the segments due to which shortening of the entire lower limb occurs (Table 2).
Table 2. – Distribution of patients by affected limb segment
| Group name | Name of the shortening segment | |
| Main group | Hip | 41 |
| Shin | 8 | |
| Control group | Hip | 42 |
| Shin | 13 | |
In the clinical practice of the Bishkek Research Center of Traumatology and Orthopedics, to determine the immediate and long-term results of lengthening large tubular bones, we used the method of standardized assessment of treatment outcomes (SOI-1) proposed by a team of authors of the Central Institute of Traumatology and Orthopedics named after N.N. Priorova (Mironov S.P., 2008).
This technique focuses on the digital assessment of outcomes, in comparison with the anatomical and functional norm (optimal functioning and development of the body). Subjective assessment of results is excluded: good, satisfactory and unsatisfactory, which does not contribute to the mathematical analysis of outcomes and does not comply with the principles of evidence-based medicine. The sum of points for all criteria constitutes an overall assessment of the anatomical and functional outcome for a given patient. The minimum possible sum of points corresponding to the worst outcome is 20. If all indicators correspond to the norm (optimal outcome), the sum of points is equal to 100 or 100% of the anatomical and functional norm (but not in comparison with a healthy limb). At the same time, it becomes possible to more accurately digitally describe the nature of the disease, eliminating verbal characteristics of the process (good, satisfactory, unsatisfactory). We modernized this questionnaire taking into account the characteristics of the subjective and objective state of patients. So we excluded point “1. PAIN” in the list of the questionnaire, since pain does not come to the fore when the limb is shortened. Instead, the item “Patient’s need for treatment at the time of examination” was introduced.
According to the criteria of the questionnaire on the 100-point SOI-1 scale, the following results were obtained in patients in the main and control groups before surgical treatment. In both groups, patients had a minimum value of 63 points and a maximum value of 73 points, the average values were 71 points (main group) and 70 points (control group). This once again confirms the identity of both groups in terms of the nature and intensity of the pathological process.
For the first time in the clinical practice of the Bishkek Research Center of Traumatology and Orthopedics, we have developed and introduced into clinical practice a method of combined lengthening of large tubular bones (invention patent KR No. 140 dated 08.19.2011, certificates for rationalization proposals No. 41/12 dated November 30. 2012, No. 45/12 dated December 4, 2012). The essence of the method is to combine two methods of osteosynthesis: a transosseous extrafocal osteosynthesis apparatus and external osteosynthesis (Figure 1).
Rice. 1. Stages of tubular bone lengthening
Under general or spinal (depending on the patient's condition) anesthesia, an Ilizarov apparatus made of half rings or full rings is applied to the limb. The rings are located at the distal and proximal levels of the tubular bone. Next, an incision is made in the skin and underlying soft tissues, the bone is exposed according to the size of the developed bone plate. An oblique or transverse osteotomy of the tubular bone is performed. A plate is applied and fixed to the proximal part of the bone with 3-4 cortical screws. The proximal bone fragment is fixed to the plate with 1-2 screws in special holes (not fixed rigidly).
Here you should indicate the technical features of the developed bone plate. The highlight of this plate is the presence in the central part of a longitudinal through groove of a certain length (depending on the planned length of the extension) for sliding the distal screws (Figure 2).
Rice. 2. Design features of the bone plate
The surgical wound is drained and sutured. We begin stretching 7-10 days after surgery; the rate of distraction depends on the type of bone being lengthened (femur, tibia, humerus) and the characteristics of the body (type of pathology, age, nature of the microelement composition of the blood). As the required limb length is achieved, under adequate anesthesia in operating conditions, final fixation of the distal tubular bone is performed with 2-3 cortical screws. The surgical incision here is much smaller and corresponds only to the length of the distal fragment. To obtain good results, it is important that the surgical technique is atraumatic and that blood circulation in the soft tissues is maintained through careful treatment of them.
In the control group, G.A. Ilizarov’s technique was used. which can be divided into three stages: osteotomy of the bone and application of the device, then distraction and, at the end, fixation of the fragments until complete ossification of the regenerate, then removal of the device. The disadvantage of this method is the long stay of the limb in the Ilizarov apparatus, until complete ossification of the bone regenerate (6-12 months), uncomfortable conditions for the patient due to the presence of a bulky apparatus in the area of the limb being lengthened. Unstable fixation of fragments and bone regenerate, the possibility of secondary mixing of fragments. High risk of wire osteomyelitis due to prolonged placement of Kirschner wires in the area of the limb being lengthened. Development of myogenic contractures of the knee joint due to the presence of the apparatus and wires in the thigh area.
Rice. 3. X-ray after implantation of the bone plate and during the lengthening process.
Rice. 4. X-ray of the lengthened segment after final fixation with screws and a completely ossified regenerate.
Results and discussion: The immediate results of treatment were studied in all 104 patients (100%), over a period of 4 to 18 months. The examination was carried out on an outpatient basis during a scheduled follow-up visit to the attending physician. During a scheduled visit, an examination was carried out and a survey card was filled out using the SOI-1 method. The examination card is a brief duplication of the medical history (basic individual data) and SOI-1 indicators in the postoperative period (after 6, 12, 18 months). Individual data were summed up, averaged, and general data characteristic for each group of patients examined was obtained, given below. In the main group, the average total score for SOI-1 was 94 points, the range was from 90 to 97 points. Whereas in the control group the average score was 81±3, and the scores ranged from 78 to 93 points. Depending on belonging to the control or main group, these results were distributed as follows (Table 3).
Table 3 - Treatment results in the control and main groups
| Results for SOI-1 | Main group | Control group | ||
| abs.h. | % | abs.h. | % | |
| From 94 to 100 points | 27 | 55.1 | 0 | 0 |
| From 90 to 93 points | 20 | 40.8 | 23 | 41.8 |
| Below 90 points | 2 | 4.1 | 32 | 58.2 |
| Total | 49 | 100,0 | 55 | 100,0 |
| Representativeness error M±σ | 16.3±12,9 | 18.3±16,5 | ||
It should be noted that in the main group the average results are 13 percent higher compared to the control group.
Based on the results of this table, we can clearly determine that in the main group, 27 patients (55.1%) had results from 94 to 100 points and in the control group (0 patients - 0%), and results below 90 points were fewer in the first group (4 .1%) by 54.1% compared to the control group (58.2%). These indicators indicate the effectiveness and adequacy of the use of improved techniques proposed by us for lengthening the long bones of the limb.
Long-term results over a period of 1-1.5 years were studied in the main group in 25 (51.1%) patients, and in the control group in 29 (52.7%) patients. This is due to various reasons (change of residence, loss of contact with the clinic). The following results were obtained: in the main group the average score was 95±3 points, and in the control group 85±3 points. Differences between outcomes in the control and study groups largely depended on the number of complications. The introduction of a new combined method of lengthening the long tubular bones of the limb made it possible to significantly reduce the number of postoperative complications and improve treatment results.
Complications in our work occurred in both the main and control groups, but differed in the severity of their manifestations and outcomes. In the main group there was 1 (3.3%) case of inflammatory complications at the site of pin wounds, but they were managed in the early stages with the use of antibiotics and local treatment (dressings, local injection with an antibiotic solution). In the control group, complications were more common and varied in severity (Table 4).
Table 4. – Nature and frequency of complications in patients in the control group
| Type of complication | Number of complications | % of total patients (n=54) |
| Suppuration of needle wounds | 2 | 3.7 % |
| Angular or transverse mixing of fragments | 6 | 11.1 % |
| Poor development of regenerate | 2 | 3.7 % |
| Pseudarthrosis, bone defect | 2 | 3.7% |
| Contractures of adjacent joints | 18 | 33.3 % |
| Total complications | 30 | 55.5% of 54 patients |
Conclusions:
- When using traditional methods of lengthening large tubular bones of a limb (Ilizarov apparatus), there are a number of structural and tactical factors that determine the occurrence of a large number of complications (wire osteomyelitis, poor development of bone regenerate, false joints and myogenic contractures).
- When lengthening large tubular bones, combining the advantages of transosseous extrafocal osteosynthesis (Ilizarov apparatus) and submersible osteosynthesis (bone plate) will significantly improve the results of lengthening during limb shortening, simplifying and adapting them to clinical conditions.
- A comparative assessment of traditional lengthening in the Ilizarov apparatus and combined lengthening using a new technique for large tubular bones of the limb showed the advantage of the latter, which consists in improving results by 13% (SOI-1).
Bibliography
- Aranovich, A. M. Rehabilitation of patients with short stature [text] / A. M. Aranovich, O. V. Klimov, K. I. Novikov // Genius of orthopedics. – Kurgan, 2011. – No. 2. – P. 15-20.
- Artemyev, A.A. Aesthetic and reconstructive surgery of the lower extremities [text] / A.A. Artemyev, Yu.G. Baranovsky, A.N. Ivashkin / ed. A.A. Artemyeva. – Moscow, 2008. – pp. 32–35.
- Bliskunov, A.I. Lengthening the femur with implanted distractors [text] / A.I. Bliskunov // In the book: medical rehabilitation of patients with bone fractures and orthopedic diseases // Collection of scientific works. - CITO. - M., 1983. - No. 26. - P. 36-41.
- Vvedensky, S.P. Pin-rod osteosynthesis in the treatment of patients with deformities and injuries of the hip [text] / S.P. Vvedensky, N.B. Tochilina, K.N. Petrushov // Modern technologies in traumatology and orthopedics: Mater, anniversary. scientific conf. - St. Petersburg, 2010. - pp. 71-72.
- Dzhumabekov, S.A. Lengthening of a congenitally shortened femur using fully implantable controlled devices “ABAS” [text] / S.A. Dzhumabekov, M.V. Andrianov, A.G. Dvorsky // Abstracts of reports. All-Union Scientific Conference of Young Scientists and Specialists. – Donetsk, 1990. – P.151-152.
- Ilizarov, G.A. The importance of tensile stress factors in the genesis of tissues and shaping processes during transosseous osteosynthesis [text] / G.A. Ilizarov // Transosseous osteosynthesis in orthopedics and traumatology: collection. scientific tr. – Kurgan, 1984. – Issue. 9. – pp. 4–41.
- Klimov, O.V. Lengthening and correction of the tibia axis [text] / O.V. Klimov, A.M. Aranovich // Modern technologies in traumatology and orthopedics: Mater. anniversary scientific conf. - St. Petersburg, 2010. - pp. 111-112.
- Sokolovsky, O.A. Option for equalizing the length of the lower limbs [text] O.A. Sokolovsky, A.I. Voronovich, I.Z. Minakovsky // Current issues. traumatology and orthopedics: mat. scientific-practical conf. traumatologists and orthopedists of the Republic of Belarus, dedicated. 70th anniversary of BelNIITO. – Minsk, 2000. – T. 1. – P. 290–294.
- Forecast of the duration of maturation of distraction regenerate [text] / N.V. Tushina, M.V. Stogov, N.A. Kononovich, A.A. Emanov // Traumatology and Orthopedics of Russia. 2012. No. 1. P. 49-54.
- Tsukanov, V.E. Method of combined distraction osteosynthesis using a blocked guide rod for lengthening long tubular bones [text] / V.E. Tsukanov, V.I. Tarasov, V.V. Vodilov // Abstract. report scientific conference - Ekaterinburg, 2007.
- Shevtsov, V.I. 24-hour limb lengthening in automatic mode [text] / V.I. Shevtsov, A.V. Popkov. – Kurgan, 2003. – P. 1–16.
- Abbaspour, A. Lengthening with external devices [text] / A. Abbaspour, S. Takata, Y. Matsui // Int. orthopedics (SICOT). – 2008. – N 32. – P. 395–402.
- Guichet, JM Gradual femoral lengthening with the Albizzia intramedullary nail [text] / JM Guichet, B. Deromendis, LT Donnan // J. Bone Joint Surg. – 2003. – Vol. 85. – P. 838-848.
- Kocaoglu, M. The methods of lengthening [text] / M. Kocaoglu, L. Eralp, O. Kilicoglu // J. Bone Joint Surg. Am. – 2004. – Vol. 86-A, N 11. – P. 2406–2411.