All achievements and victories lose meaning if a man is not able to fully express himself in the intimate sphere of his life. A sexual life filled with vivid sensations and the ability to satisfy the woman you love are the best proof of your own masculine essence.
However, many have to deal with various problems: from purely aesthetic defects, congenital defects of the genital organs that prevent the ability to perform full sexual intercourse, to impotence. This certainly leads to despair and sometimes causes deep depression when life seems in vain. In such cases, male intimate plastic surgery comes to the rescue, the possibilities of which today are almost limitless.
Treatment of impotence
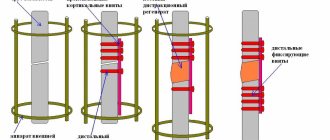
Male intimate plastic surgery offers treatments for erectile dysfunction that provide 100% erection and can significantly improve the quality of sex. For example, you will be able to decide for yourself how long sexual intercourse will last. This opportunity opens up, in particular, thanks to the implantation of penile prostheses: they are completely invisible visually, so your partner will have no reason to doubt your masculine strength.
Male plastic surgery of the intimate area allows not only to preserve the fullness of orgasm and sensations from sexual intercourse, but can also make them more colorful. The surgical intervention is carried out under general anesthesia: penile prostheses are implanted into the cavernous bodies of the penis, which are selected in accordance with its anatomical features.
Penis extension
To date, there is no standard for penis length. However, if in an erect state the organ does not reach at least 12 cm, this can become a source of problems and psychological pressures. Nowadays, penile lengthening surgery is one of the most requested procedures in the field of intimate plastic surgery for men. With its help, it is possible to lengthen the penis by 2-5 cm. The intervention is carried out under anesthesia, and the patient first undergoes a series of preoperative examinations. Staying in the hospital requires no more than a day; on the second day the person can return to normal life. To achieve a successful result, it is extremely important to follow all recommendations from the doctor.
Postoperative period
After discharge, it is necessary to limit physical activity for 1 month, and also perform dressings for some time.
During the entire recovery period after surgery (about one month), it is necessary to refrain from sexual activity in any form, including masturbation. At the end of the recovery period, the man can return to intimate life in full.
Possible complications and contraindications will be discussed with you individually by your attending physician.
Penis thickening
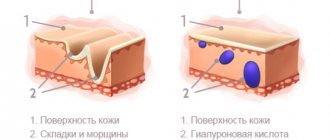
The need to increase the size of the penis often arises among men who know first-hand how important high-quality sexual contact is. If the penis is really far from perfect or simply the size of the partner’s vagina does not allow achieving maximum mutual satisfaction, you should think about thickening the penis. It is performed using the lipofilling method, when one’s own fat cells are used to increase natural size.
An alternative to adipose tissue is a special gel. This type of male intimate plastic surgery has a short rehabilitation period and does not require you to stay in a hospital: literally in half an hour you can go home, and after 3 days you can evaluate the result in practice.
Another way to thicken the penis is to transplant muscle tissue taken from the abdomen, which is evenly located under the skin of the penis, wrapping it along its entire length. This method will require a slightly longer rehabilitation period.
The specific method of penis thickening is determined for you individually and guarantees the achievement of your desired result.
Features of other plastic surgeries in men
Plastic surgery for men is not limited to intimate plastic surgery. Listed below are the most popular aesthetic surgeries among the stronger sex and their features, which the surgeon takes into account at the stage of planning the correction and during the implementation of the intended strategy.
Blepharoplasty
A common “male” problem is bruising or bags in the lower eyelid area. Due to existing stereotypes in society, they are strongly associated with the abuse of strong drinks, although in reality the owner of bags under the eyes may be a convinced teetotaler.
The problem is solved with lower blepharoplasty. The operation is performed through classic (skin incisions) or transconjunctival (no skin incisions) access. Healing proceeds quickly, and the results of eyelid surgery last for many years. Upper blepharoplasty is performed much less frequently on men, since slight drooping of the upper eyelids is typical for male facial features.
Rhinoplasty
Male nose surgery is more often performed in an open manner, since men are not embarrassed by small scars on the skin in the nostril area. Men's skin tends to be thicker, making open access difficult. In addition, men often turn to a plastic surgeon after sports or everyday fractures, and nasal reconstruction is performed mainly in an open manner.
A plastic surgeon has to take into account many nuances when assessing the indications for nose surgery. For example, for men, a slight drooping of the tip or a slight hump is a normal option, which most often does not require correction. But an upturned nose is always an aesthetic problem.
Mentoplasty
Another male surgery is chin surgery. The need for it arises in cases where the chin is underdeveloped, appears small against the background of the overall proportions of the face, or has a slanted shape. Since such appearance features are in no way associated with masculinity, patients turn to a plastic surgeon for help.
Correction of the shape of the chin is carried out using the installation of implants. A cartilage implant (from the patient’s own cartilage tissue) or a synthetic one made from medical polymers is sutured to the mandibular bone. Less commonly used is lipofilling, which we have already discussed. The result of the operation remains for life, which compensates for the minor limitations of the rehabilitation period.
Liposuction
There are no particularities in performing liposuction in men; they are characterized only by the specific localization of problematic fat deposits. If in women excess fat is distributed mainly in the area of the gluteal complex and hips, then in men the aesthetics of the lower abdomen primarily suffers. Abdominal liposuction is a very common plastic surgery procedure for men.
Gynecomastia removal
Another purely male operation is the removal of pathologically hypertrophied mammary glands. The cause of gynecomastia may be the use of androgenic anabolic steroids (typical for athletes) or hormonal disorders accompanied by an increase in estrogen levels.
The aesthetic problem is solved with the help of surgery. Removal of gynecomastia is a simple operation and does not require complex rehabilitation. It is important to understand that eliminating a symptom does not eliminate the cause of its occurrence. The patient needs to undergo an examination, determine the root cause of the hormonal imbalance and take measures aimed at normalizing hormone levels.
Hair transplant
This aesthetic medicine procedure successfully copes with the problem of male pattern baldness. Hair follicle transplantation gives a 100% result that lasts for many years. Sometimes patients turn to a plastic surgeon to transplant facial hair and become the owner of a luxurious mustache or beard.
Cruroplasty
Many men, including athletes, are interested in shin surgery. This is explained by the fact that the calf muscles respond extremely poorly to growth stimuli generated during strength training. To improve the aesthetics of their legs and achieve ideal proportions, some athletes resort to surgery.
In recent years, other surgeries aimed at modeling body contours and recreating athletic proportions have become popular among men. The operation to create outstanding “abs” is quite in demand. Some men use implant placement (or lipofilling) to create ideal contours of the pectoral muscles.
Modern plastic surgery opens up limitless horizons of possibilities for modeling the body, eliminating deficiencies, and creating ideal proportions for a successful man. You can learn more about the possibilities of aesthetic medicine during a consultation with a plastic surgeon at the Moscow Soho Clinic.
Male intimate plastic surgery: enlargement of the head of the penis
The head of the penis is usually larger in diameter, but in some cases its dimensions clearly do not correspond to the “standard”. A visible visual discrepancy is possible, for example, after an operation to increase the volume of the penis, when the size of the head remains the same. The medical procedure for thickening the head of the penis is carried out as follows: under local anesthesia, a special gel is injected into the head, which is evenly distributed inside. Recovery is very fast. In just 3 days you will be able to resume your sex life.
Reconstructive genital plastic surgery for giant elephantiasis of the external genitalia in men
M.N. Tillyashaikhov, E.V. Boyko, N.T. Rakhimov, L.P. Root, Sh.T. Khasanov, N.T. Abdusamatov, A.Kh. Otaboev
Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan
A wide range of doctors in everyday clinical practice sometimes encounter so-called “rare diseases”, the diagnosis, treatment and long-term results of which are little known. It is often impossible to find generalizing information in the literature about such diseases; presents great difficulty, and treatment results remain unsatisfactory. Therefore, you have to spend a lot of time and effort searching for the causes of these pathologies.
“Rare disease” is a subjective and vague concept. In this regard, there was a desire to share a “rare” observation on the pages of specialized magazines.
Lymphedema of the scrotum is a rare pathology associated with impaired lymph outflow, also known as elephantiasis (elephantiasis) [1-6]. Violation of the drainage system of the scrotum develops against the background of filariasis in a parasitic form with a congenital pathology with an anomaly of lymph collectors, and also progresses secondarily with chronic sexually transmitted infections and after injury [7-10]. Occurs in 0.01% of urological patients [11]. The progression of the disease leads to a significant change in the volume of the genital organs [12]. The size of the affected area increases significantly, the skin thickens, hypertrophies, becomes lumpy and covered with non-healing ulcers [13-15]. Patients suffering from this pathology complain of the inability to maintain adequate genital hygiene, pain, and difficulty moving [16,17]. This physical condition determines a decrease in the patient’s psychosomatic status. Surgical removal of hypertrophied scrotal skin, fibrously changed subcutaneous tissues with various options for reconstructive plastic surgery of the external genitalia is one of the treatment methods that improves the quality of life of patients [18-24].
Most researchers in the CIS and abroad have only isolated observations. The majority of these patients have a low psychosomatic status and therefore remain only under dynamic observation.
The purpose of the article is to report on a patient with giant scrotal lymphedema, who underwent surgical treatment of this pathology for the first time in Uzbekistan and observed its immediate results.
1 Patient Kh.Sh, aged 21 years, was treated in the urology department of the Republican Scientific and Practical Medical Center from 04/24/2018 to 05/14/2018.
Upon admission, he complained of an increase in the size of the scrotum, difficulty urinating, difficulty walking (the scrotum interfered with walking), inability to have sexual activity, swelling of the left arm, and weakness.
History: Sick since childhood. Enlargement of the scrotum was noticed in 2010. After contacting a specialist, he was sent to the Republican Specialized Center for Surgery named after Vokhidov, where on August 30, 2010, a scrotoplasty operation was performed. From the surgical protocol it was revealed that at the time of the operation the scrotum had a size of 25x18 cm. 5 months after the operation there was a repeated increase in the size of the scrotum. The patient again applied to the Republican Specialized Surgery Center (RSSC) on June 2, 2011 for repeated surgical treatment, but was discharged due to family problems. From that moment on, the patient underwent an annual medical examination at his place of residence. Over time, the patient began to notice an increase in the size of the scrotum, so he returned to the RSCC, but the patient was denied treatment. The patient applied to several medical institutions, but, unfortunately, treatment was denied there too. Motivated by the lack of specialists in this field, the patient was redirected to the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology (RSNPMCOiR) where he was examined in the conditions of the oncourology department. At the stages of the examination, helminthiasis “wuchereriosis” was suspected and was sent to the Research Institute of Parasitology. After ruling out helminthiasis, the patient returned to the RSNPMTSOR.
Objectively: General condition is satisfactory, active. Peripheral lymph nodes are not enlarged. The stomach is soft. Locally: the left elbow is swollen. The external genitalia cannot be palpated, as there is swelling of the skin of the scrotum and pubic area. The size of the scrotum is 80x90 cm, localized in the perineum, deforming the skeleton of the lower extremities. The penis is lost in the folds of the skin of the scrotum (Fig. 1). Urination is voluntary. There is maceration of the skin of the scrotum with urine.
Rice. 1 (A-B) Front and rear view 1 (AB) Frontal and posterior view
SURVEY METHODS
Chest X-ray (04/27/2018): Right lung without shadows. The intercostal spaces are symmetrical. On the left, in the lower pulmonary field, a single rounded shadow of low intensity with smooth contours, up to 1.0 cm in diameter, is determined. The roots of the lungs are compacted.
Heart shadow without features. The pleural sinuses are free.
Multislice computed tomography: (October 24, 2017) Axillary lymph nodes up to 1.1-1.3 cm, mediastinal lymph nodes, bronchopulmonary nodes are clearly not enlarged; at the level of the diaphragm on the left there is a node with a diameter of 1.2 cm. In the parenchyma of both lungs there are separate small subpleural infiltrative strands. Moderate hepato-splenomegaly. Retroperitoneal nodes up to 1.0 cm. Massive swelling of subcutaneous fat at the level of the walls of the abdominal cavity and pelvis, swelling extends to the tissue of the chest walls. There is an increase and thickening of the parenchyma of both mammary glands. At the level of the perineum and scrotum, the formation of a heterogeneous structure is determined, measuring 42.0x22.0x36.0 cm, coming from the organs of the scrotum. There is pronounced swelling of the subcutaneous fat at the level of the pelvic floor and lower extremities. Ileac nodes up to 1.2 cm, inguinal nodes against the background of edematous tissue are not differentiated separately (Fig. 2).
Rice. 2. (A-B) MSCT of the area of interest: sagittal and axial sections, pronounced swelling at the perineal level, enlargement of the scrotum, the structures of the scrotum are not determined separately. Fig. 2. (AB) (AB) MSCT regions of interest: sagittal and axial slices, apparent edema at the level of the perineum, an increase in the scrotum, the structures of the scrotum are not defined separately
Tumor markers (04/28/2018): Alpha-fetoprotein (AFP) – 1.2 U/ml (normal: 0-10), lactate dehydrogenase (LDH) – 276.8 U/l (normal: 225-450), chorionic gonadotropin (CG) – 1.4 IU/l (normal: up to 15).
Doppler ultrasound (USD) (April 27, 2021): On echotomograms: liver - oblique vertical dimension (OVD) of the right lobe 146 mm (normal), craniocaudal (OCD) of the left lobe - 93 mm (normal). The contours are clear and even. Parenchyma of increased echogenicity, fine-grained, at the border of 7-8 segments of homogeneous increased echogenicity, a node with clear contours of 15x14x14 mm is determined. In the 7th segment of a similar structure there is a 10x8 mm inclusion. With color Doppler mapping, intranodular vascularization is not visible. The intrahepatic bile ducts are not dilated. The diameter of the hepatic veins is 7 mm (normal), the diameter of the portal vein is 10 mm (normal). Conclusion: focal inclusions in the right lobe of the liver (capillary hemangiomas).
The patient underwent the operation “Scrotectomy, scrotoplasty from local tissues” as planned on May 23, 2018.
The first step was to mobilize both testicles. A 15 cm long skin incision was made on the right side parallel to the inguinal fold. Hemostasis. During mobilization of the testicle, a large volume of lymphatic fluid was released from the adjacent tissue. The subcutaneous adipose tissue is thickened to 10 cm. With technical difficulties, it was possible to find the aponeurosis. The latter is dissected and the spermatic cord is discovered, it is taken on a tourniquet and, focusing on it, the testicle is isolated using a sharp and blunt method (there was a history of surgery on the right testicle). The adhesive process and the size of the testicle made it impossible to release it into the wound. In this regard, it was decided to approach the testicle from the outside: an incision was made in the skin of the scrotum. During mobilization, the testicular membrane was opened, and 1.5 liters of clear yellowish liquid (dropsy) was released. Due to technical difficulties, the testicle was isolated into the wound along the groin line. A similar operation was performed on the left. In this case, the volume of liquid was 2.0 liters. Both testicles were treated according to the Bergmann operation.
The next stage is the mobilization of the penis. Due to swelling of the tissues adjacent to the penis and lymphostasis, a tunnel 10 cm deep was formed, from which urine flowed. After opening the tunnel under finger control, the head of the penis was discovered. The bladder was immediately catheterized with a transurethral catheter. Under the control of a finger and a transurethral catheter, the shaft of the penis is mobilized. The large mass of the scrotum is cut out along conventionally drawn lines. Hemostasis has been completed. Both testicles are placed in a formed scrotum, formed from surrounding tissues, and drained. Plastic surgery of the defect was performed from surrounding local tissues. The wound is treated with antiseptic solutions (Fig. 3-10). an aseptic dressing was applied. Macroscopic specimen: the removed scrotum measured 80x70 cm, the operating period proceeded smoothly. The drains were removed on day 8 (Fig. 12). The sutures were removed on the 13th day after surgery (Fig. 13). He took psychosomatic rehabilitation courses. The patient fully recovered and returned to normal life without complexes (Fig. 14). The sexual function of the reproductive system organs is not impaired.
Rice. 3. Stage of mobilization of the spermatic cord on the right 3.Stage of the spermatic cord mobilization on the right
Rice. 4. Mobilization of the right testicle 4. Right testis mobilization
Rice. 5. Hydrocele of the right testicle 5. Right hydrocele
Rice. 6. The testicular membrane is opened 6. Testis coat opened
Rice. 7. Performing the Bergman operation stage 7. Von Bergman's operation stage
Rice. glans penis 8. Balanus extraction and mobilization
Rice. 9. Plastic surgery of the skin of the penis 9. Plastic reconstruction of the penis skin1
Rice. 10. Removal of scrotal mass 10.Dissecting out of scrotal mass
Rice. 11.Macropreparation. Fig. 11. Gross specimen
Fig. 12. View of the wound after surgery Fig. 12. After surgery wound view
Rice. 13. 15 days after surgery Fig. 13. 15th day after surgery
Summary: Lymphostasis of the penis and scrotum is a rare pathology in our region. In cases of severe disease, surgical treatment is the treatment of choice to improve the patient's overall quality of life. This case is interesting because surgery was used to treat huge scrotal lymphostasis, which led to an improvement in the patient’s quality of life.
Rice. 14. 3 months after surgery 14. 3 months after surgery
CONCLUSIONS
An attempt was made to find possible ways of rational surgical treatment, taking into account the rarity of the disease. The main thing in diagnosis and treatment, according to V.A. Oppel “remember that it is and exists.” The team of authors expresses the hope that his work will be useful for doctors.
To perform this volume of surgery requires the synchronized work of surgeons, anesthesiologists, transfusiologists, as well as enormous physical labor, psycho-emotional endurance and professionalism of each doctor.
LITERATURE
- Lee S, Han JS, Ross HM, Epstein JI. Massive localized lymphedema of the male external genitalia: a clinicopathologic study of 6 cases. Hum Pathol 2013;44(2):277-81. doi: 10.1016/j.humpath.2012.05.023.
- Mukenge SM, Negrini D, Catena M, Ferla G. Innovative microsurgical treatment of male external genital lymphedema. World J Clin Urol 2014;3(3):310-319. doi: 10.5410/wjcu.v3.i3.310.
- McDougal WS. Lymphedema of the external genitalia. Urol 2003;170(3):711-716. doi: 10.1097/ 01.ju.0000067625.45000.9e.
- Modolin M, Miter AI, da Silva JCF, Cintra W, Quagliano AP, Arap S, et al. Surgical treatment of lymphedema of the penis and scrotum. Clinics 2006;61(4):289-94. doi: 10.1590/S1807-59322006000400003.
- Kulungowski AM, Schook CC, Alomari AI, Vogel AM, Mulliken JB, Fishman SJ. Vascular anomalies of the male genitalia. J Pediatr Surg 2011;46(6):1214–21. doi: 10.1016/j.jpedsurg.2011.03.056.
- Lopatkin N.A., Sivtsev V.V., Safarov R.M. Elephantiasis of the external genitalia. In the book. Selected lectures on urology [Under. Ed. ON THE. Lopatkina, A.G. Martova]. Medical Information Agency, M.; 2008.S. 560-573. . Medical News Agency, M.; 2008.S. 560-573. (In Russian)].
- Halperin TJ, Slavin SA, Olumi AF, Borud LJ. Surgical management of scrotal lymphedema using local flaps. Ann Plast Surg 2007;59(1):67-72. doi: 10.1097/01.sap.0000258448.17867.20.
- Vignes S, Trévidic P. Lymphedema of male external genitalia: a retrospective study of 33 cases. Ann Dermatol Venereol 2005;132(1):21-25. doi: 10.1016/s0151-9638(05)79190-0.
- Baumeister RGH, Siuda S. Treatment of lymphedemas by microsurgical lymphatic grafting: what is proven? Plast Reconstr Surg 1990;85:6474; discussion 75-76. doi: 10.1097/00006534-199001000-00012.
- Franco Mora MC, Pichín Quesada A, Giraudy Simón G, León Estrada M, Candebat Montero LH, Tamayo Tamayo I. External genitalia lymphedema. Case report. Arch Esp Urol 2007;60(6):688-692. doi: 10.4321/s0004-06142007000600012.
- Favager N, Rist M, Krupp S. Reconstruction cutanée des organes genitaux externes: une ancienne méthode toujours d'actualité. Helv Chir Acta 1991;58:301-3.
- Sun GS, Zhong AG, He W, Du P, Song WM, Ma JG. Reconstruction of the external genitals and repair of skin defects of the perineal region using three types of lateral groin flap. Ann Plast Surg 1990:24:328-34. doi: 10.1097/00000637-199004000-00005.
- Nelson RA, Alberts GL, King LE Jr. Penile and scrotal elephantisis caused by indolent. Chlamydia trachomatis infection. Urology 2003;61(1):224. doi: 10.1016/s0090-4295(02)02078-2.
- Mikhailichenko V.V., Fesenko V.N. Clinical observation of isolated elephantiasis of the penis. Andrology and genital surgery. 2013;14(3):58-60.
- Elkiran YM, Elshafei AM, Abdelgawwad MS, Abdelmaksoud MA. Surgical management of giant scrotal lymphedema in morbidly obese patient with trisomy 21 J Vasc Surg Cases Innov Tech 2019;5(1):71-74. doi: 10.1016/j.jvscit.2019.02.002.
- Liang L, Aftab-Hashmi M, Mirsaeidi H. Treatment Program for the Management of Acute Male Genital Edema/Lymphedema. J Hosp Med Manage 2017;2:12. doi: 10.4172/2471-9781.100031.
- Qing L, Zhaohua J, Zizhou Z, Lianming W, Guangyu W, Shiteng S, et al. Assessment of The Lymphatic System of the Genitalia Using Magnetic Resonance Lymphography Before and After Treatment of Male Genital Lymphedema. Medicine 2016;95(21):3755. doi: 10.1097/ md.0000000000003755.
- Rahman GA, Adigun IA, Yusuf IF, Aderibigbe AB, Etonyeaku AC. Giant scrotal lymphedema of unclear etiology: a case report. J Med Case Rep 2009;3(1):7295. doi: 10.1186/1752-1947-3-7295
- Garaffa G, Christopher N, Ralph DJ. The management of genital lymphoedema. BJU Int 2008;102(4):480–484. doi: 10.1111/ j.1464-410X.2008. 07559.x.
- Denzinger S, Watzlawek E, Burger M, Wieland WF, Otto W. Giant scrotal elephantiasis of inflammatory etiology: a case report. J Med Case Rep 2007;1:23. doi:10.1186/1752-1947-1-23.
- Mukenge SM, Catena M, Negrini D, Ratti F, Moriondo A, Briganti A et al. Assessment and follow-up of patency after lymphovenous microsurgery for treatment of secondary lymphedema in external male genital organs. Eur Urol 2011;60(5):1114–1119. doi: 10.1016/ j.eururo.2010.11.020.
- Parmar HD. The surgical approach in huge scrotal lymphedema. Int J Med Sci Public Health 2013;2(1):153-155. doi: 10.5455/ ijmsph.2013.2.153-155.
- Kurbatov D.G., Dubsky S.A., Lepetukhin A.E., Gorokhov M.A., Shvarts Ya.G. Method for treating scrotal elephantiasis with free autodermal flaps (clinical observation). Andrology and Genital Surgery 2012;13(3):107-109. .
- Safarov R.M., Sivtsev V.V., Efremov E.A., Polyakov N.V., Verzin A.V. Surgical treatment of genital elephantiasis in men. Abstracts of reports of the XIX Congress of the Russian Society of Urologists. Rostov-on-Don, September 19-21, 2021 pp. 66-67. .
The article was published in the journal “Experimental and Clinical Urology” No. 4 2021, pp. 114-120
Topics and tags
Open surgery in urology
Magazine
Journal "Experimental and Clinical Urology" Issue No. 4 for 2019
Comments
To post comments you must log in or register
Correction of penile curvature
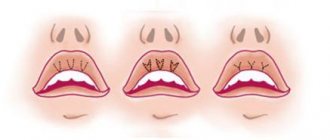
The curvature of the penis is its significant deviation in any direction (the level of bending is more than 60 degrees). The pathology becomes most noticeable during erection and can lead to unpleasant sensations during sexual intercourse. Curvature can be congenital or acquired (as a consequence of Peyronie's disease). In the second case, deformation of the tunica albuginea of the penis occurs, which slowly but surely causes and intensifies pain during sex.
The field of intimate plastic surgery for men offers effective methods of treating a “crooked” penis, thanks to which you can quickly return to a full sexual life. Surgical intervention involves placing longitudinal sutures on the tunica albuginea of the organ. Literally in 7-10 days you will be able to practically evaluate the effect, forgetting about the pain during sexual intercourse forever.
Indications for intimate correction?
The appearance and functionality of the genital organs is of great importance for a person; not only the degree of sexual satisfaction, but also general psychological comfort depends on this.
In a word, complexes disappear, self-confidence increases. With age, due to various influences, both external and internal, due to the individual characteristics of the body, the condition of the genital area may worsen. The traditional way to correct the situation is surgery. Many patients are not ready to take such a radical step or have serious contraindications. In this case, of course, modern non-surgical techniques become the optimal solution. They allow a specialist to solve many aesthetic and even functional problems absolutely painlessly and for a fairly long period - from six months to one year.
Men can resort to these procedures if they have the following problems:
- Premature ejaculation;
- Dissatisfaction with the size and shape of your penis.
Specialists from the Clinical Institute of Regenerative Medicine will help you solve your problems!
Non-surgical intimate correction for men can be performed in the following cases:
When eliminating premature ejaculation
- According to statistics, rapid ejaculation is a problem that up to 50% of men periodically or constantly face. Injections of fillers based on hyaluronic acid or the use of plasmogel are currently considered the simplest and least traumatic method of solving this problem. The filler is injected into the area of the frenulum and coronal sulcus of the penis, which increases the distance between the sensitive genital receptors and the surface layer of the skin. As a result, the duration of sexual intercourse increases markedly. Over time, the filler dissolves, but the psychological attitude towards long-term sexual intercourse can be preserved, and new injections will no longer be needed.
Plasmolifting has also been proven to have a positive effect on erectile function in men.
Changing the size and shape of the penis
Justified or subjective dissatisfaction with the size of one's penis, the presence of curvatures and other defects creates severe discomfort in most men, which can lead to serious functional problems, including impotence. Injections into the soft tissues of the penis allow you to correct its shape, increase the size of the head, etc. Unfortunately, intense friction during sexual intercourse leads to rapid resorption of fillers, so experts do not consider this technique to be quite effective, but it is the most gentle method for solving a number of aesthetic and functional problems.
Plastic surgery of the frenulum of the foreskin
The normal functioning of the frenulum of the penis is the key to a quality sexual life, since it is responsible for the movements of the foreskin when the head of the penis is exposed. Problems arise with a very short frenulum - in this case, sexual intercourse causes pain and provokes microcracks and tears in it. To solve such problems, a type of intimate plastic surgery for men is used, such as frenuloplasty, which allows you to increase its length.
A short procedure restores the normal functioning of the frenulum, and the postoperative period lasts no more than 2-3 weeks. If you are experiencing premature ejaculation, this procedure may help. The fact is that with a short frenulum, ejaculation is faster than in those who have a normal frenulum length. You will not need to stay in the hospital after the intervention: you can sign up and carry out the procedure without interrupting your usual rhythm of life.
Postoperative rehabilitation
The duration of rehabilitation depends on the complexity of the operation, the type of intervention and the patient’s health condition. Depending on the type of intervention, the patient may go home immediately or remain in the hospital for some time. The specialist may recommend taking medications, dressings, and a diet to speed up the healing process.
The cost of the operation depends on the complexity of the surgical intervention, the number of additional diagnostic measures, dressings, etc. To make an appointment with our specialists at Delta Clinic and find out the price of treatment, call the contacts listed on the website.
Circumcision (circumcision)
The operation of excision of the foreskin is performed not only on men who undergo it for religious reasons. First of all, this type of intervention is carried out to treat phimosis, which we wrote about above. The procedure also has a number of advantages, for example:
- reducing the risk of developing genital cancer;
- prolongation of sexual intercourse by reducing the sensitivity of the head of the penis.
The operation is performed under general or local anesthesia. After it, minor stitches remain, but they dissolve on their own. The rehabilitation period takes 2-3 weeks, during which the patient is prohibited from physical activity, sex, and sauna.
Testicular prosthetics
The absence of a testicle(s) can be caused by a number of factors, with the main causes of this problem being previous surgery for medical reasons or serious injuries. Intimate plastic surgery for men in Novosibirsk at the Dune Ego clinic allows you to level out this aesthetic drawback by implanting a prosthesis that follows the natural anatomical shape of the testicle. Surgery is performed under local or general anesthesia. Afterwards, the recommended stay in the hospital is from 2-3 to 24 hours. In just 3-4 days you will be able to return to your sexual life.