Stages of the operation. Photo
Nose surgery – Rhinoplasty. We present to your attention a photo session of rhinoplasty surgery
Before surgery
Examination of the nasal passages
Marking before surgery
Hydropreparation
Soft tissue dissection
Tissue mobilization
Tissue mobilization
Soft tissue detachment
Isolation of the “wing” cartilages of the nose
Isolation of the “wing” cartilages of the nose
Excision of the “wing” cartilages of the nose
Excision of the “wing” cartilages of the nose
Forming a “support” for the tip of the nose
Removal of nasal hump
Shaping the tip of the nose
Suturing the edges of the wound
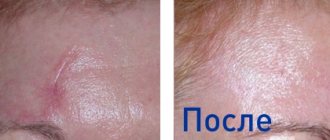
After operation
What shortcomings can be corrected?
Non-surgical rhinoplasty cannot radically change the shape of the nose, but is guaranteed to help with:
- asymmetrical shape of the wings and curvature of the back;
- the presence of unwanted depressions and dips;
- hump;
- unsuccessful rhinoplasty;
- drooping of the tip of the nose;
- flattening of the back;
- sagging skin;
- correction of the consequences of injury.
Fillers act as implants: they add volume in the right places, thereby correcting imperfections and hiding flaws.
The result of non-surgical rhinoplasty
Aesthetic rhinoplasty (nose job) – correction of the size and shape of the nose.
Rhinoplasty is a plastic surgery aimed at changing the shape and/or size of the external nose. The goal of rhinoplasty is to create a new harmonious appearance, while maintaining individual characteristic facial features. Nasal deformities can be congenital or acquired (trauma, previous surgeries, burns, etc.). Visible deviations from the norm are manifested by either excess or deficiency of tissue, deviations in the position, shape, symmetry and size of the nose. Even a small correction of the nose can significantly change the appearance of the face and rid a person of uncertainty and complexes. Rhinoplasty (nose job) involves:
- nose reduction;
- removal of the nasal hump;
- correction of a crooked nose;
- correction of a deviated nasal septum;
- correction of the tip of the nose (wide, protruding or sagging);
- elimination of saddle nose deformation.
All operations are performed under general anesthesia using local anesthesia, and are completely painless for the patient.
Rhinoplasty can be performed after the patient reaches 18 years of age, when the facial skeleton completes its formation. The most suitable age for performing aesthetic rhinoplasty is the period from 20 to 35-40 years.
And since modern rhinoplasty technologies do not leave traces of the operation on the skin, patients return to their usual surroundings, as if nothing had happened, after 9-15 days.
Rhinoplasty: from start to finish
Introduction or brief historical overview
Everyone knows that humanity's historical obsession with beauty and the inexhaustible resource of surgical technology that faithfully serves us today are based not least on the sinful vanity of the 16th century, when Europe was swept by an epidemic of syphilis. It was then that Chirurgiadecoratoria (Aesthetic Surgery) appeared, trying to restore sunken noses so that the indecent disease would not be so obvious to others. Surgeon Gaspare Tagliacozzi from the University of Bologna was the first to see the connection between a physical defect (nose) and the self-perception of such patients (and told it to the world in pictures: in 1597, in the illustrated treatise “De Curturum Chirurgia per insitionem” - a technique for reconstructing a nose lost as a result of syphilis , using skin flap transplantation). I would call this period the period of the greatest sexual tragedy, when the suffering, troubles and inconveniences caused by the disease, and subsequently complete rejection by society, significantly outweighed the instant bursts of pleasure on the scales of happiness. Tagliacozzi invented a method (not worthy of abstinence) with which it was possible to “grow” a new nose in place of the lost one. Today, looking through punctual notes + pictures from surgical atlases of that time (I can’t help thinking that they remind me of surgical comics), you understand how courage, patience (both on the part of surgeons and patients) and drama permeated the entire path that I have had rhinoplasty since then. Strategically, it developed in two different directions - correction of external deformations and restoration of internal structures of the nose (septum, turbinates) to ensure normal breathing functions. The surgeon J.F. Dieffenbach (1792-1847) developed provisions sufficient to become the basis, the basis of all modern rhinoplasty. He proposed and described operations for noses with a wide dorsum, long noses, and noses with an osteocartilaginous hump, using external, median or lateral approaches. However, a little later, otolaryngologist J. O. Roe (1849-1915), who had a greater understanding of the values of aesthetics and the absence of scars, considered external incisions for rhinoplasty to be old-fashioned and suggested the use of endonasal (internal) ones. R.V. Veer (1838-1927), a surgeon with an innovative approach, was the first to perform a lateral osteotomy, which has not become a relic today, as well as partial resection of the wings of the nose to narrow them, which became a real breakthrough in rhinoplastic creativity. Surgeon Mr. J. Joseph "designer" experimented with wing cartilage. He introduced a number of new tools, demonstrating a better understanding of surgical comfort and its role in achieving better results.
Goals of rhinoplasty
Let's leave historical irony behind and move into the modern world of rhinoplasty or nose shape correction, which is one of the most popular operations in plastic surgery. The nose can be reduced, enlarged (using your own cartilage or special implants), change the angles - nasolabial (between the columella and upper lip) and profile (between the nasal bones and forehead), straighten in the front, make the bridge of the nose narrower, etc., but the most common requests from patients are:
- raise and (or) rotate the tip of the nose, shorten it and make it narrower in front (sometimes with partial resection of the wings of the nose);
- remove the osteochondral hump and lower the projection of the nasal dorsum, respectively making the nasal dorsum straight or slightly concave in profile and aligned to the front (for asymmetry associated either with a deformation of the nasal septum or after a nasal injury).
An aesthetically harmonious appearance of the nose must correspond to the general proportions of the face and body and is unique in each anthropometric case (racial characteristics, state of occlusion, etc.). The favorites of “nasal” beauty are those with “Scandinavian genetics” with straight backs and narrow tips. In our practice, it is reduction rhinoplasty that occupies a leading position. In preparation for surgery and to assess future changes, computer modeling (usually in a profile projection) of the nose is performed, which helps both the patient and the surgeon to imagine, firstly, the desired and, secondly, the surgically possible variant of changes. After that, the surgeon is required to do only one thing - to transfer to the operating room and implement in the surgical technique the amazing world of changes in the nose that emerged during the discussion and depicted during modeling.
Indications for surgery
The main reason patients turn to plastic surgery clinics is to reduce the entire nose or its individual parts. To understand the scope of the upcoming rhinoplasty, the surgeon evaluates both the profile projection and the front view of the nose (in profile, the subnasal and profile angles are well visualized and conveniently interpreted, assessing which one can judge the excess length of the nose, which means one can quite accurately predict the degree of shortening of the nose). To change the forward projection (fas), narrowing of the tip and dorsum of the nose, as well as shortening of the columellar part of the tip, is usually performed. The degree of narrowing should be consistent with the aesthetic views of both the patient and the doctor, and generally the width of the tip of the nose should be twice (or so) the width of the bridge of the nose, and the nostrils should not project significantly beyond the lines descending vertically from the inner corners of the eyes.
Key stages of reduction rhinoplasty technique
1. Frenuloplasty (plasty of the frenulum of the upper lip or a method of lengthening it).
Frenuloplasty is most often performed using the VY method of plastic surgery of the mucous membrane of the upper lip with subperiosteal separation of the muscle that depresses the ala of the nose. The goal of frenuloplasty is to eliminate the vector effect on the tip of the nose, which is especially noticeable when the muscle group in the area of the upper and lower lips is reduced. For example, when smiling or during a conversation in such patients, the tip of the nose moves up and down, which gives individual piquancy to its owners, but for rhinoplasty it is important that this vector stops influencing the tip of the nose and does not interfere with the surgeon’s “rotation” of it to an aesthetically desired position .
2. Septoplasty (plasty of the septal cartilage in case of its deviation).
In the presence of deviation (curvature) of the nasal septum, partial gentle resection of the curved sections of the cartilaginous and bone parts of the septum is most often performed. Care must be taken not to remove the septal cartilage too high (close to the skin) - this can lead to unpredictable changes in the nasal bridge in the future. If necessary, the surgeon performs conchotomy or coagulation of the nasal turbinates. The presence of a deviated nasal septum can cause not only difficulty breathing, but also deviation (deviation along the vertical axis of the nasal dorsum to the right or left), for the elimination of which septoplasty is a necessary step
3. Shortening the tip of the nose (in most rhinoplasties, a particularly important point when shortening the tip of the nose is its rotation or turning counterclockwise to change the nasolabial angle, which should be equal to 105 * -110 *). Nasal shortening aims to increase the nasolabial angle and is achieved through a bilateral full transfection incision. In order for the tip of the nose to simply become higher, it is necessary to excise a uniform strip of the distal edge of the septal cartilage. If it is necessary for it not only to become higher, but to turn upward or “rotate” in the upper part, it is necessary to additionally excise a small section of the septal cartilage precisely in the upper part of the tip of the nose.
4. Narrowing of the alar cartilages and, if necessary, lowering the projection of the tip of the nose.
Through marginal access on the right and left, the wing cartilages are isolated using the luxation (dislocation) method. A number of surgeons also use intercartilaginous incisions to facilitate luxation of the alar cartilages. The alar cartilage is changed by removing the cephalad (upper) sections of the lateral crura, and, if necessary, reducing the projection of the tip of the nose by resection of sections of the alar cartilage from the area of the arches. If this is not enough, then a transverse strip is excised from the lateral crura of the alar cartilages closer to the base of the nasal wing and away from the arches. After assessing the symmetry of the remaining parts of the lateral crura, they are stitched with catgut 5.0. The tip of the nose is formed.
5. After removal of the periosteum and perichondrium, resection of the osteochondral hump with correction of the septal angle.
First, the bony part of the hump is removed with a direct osteotome, then the cartilaginous part is sharply removed, followed by processing of the irregularities with a rasp. The transition zone of the nasal dorsum to the tip, the so-called septal angle, is treated separately; most often, a small section of triangular-shaped cartilage is resected to prevent the appearance of a hump in the supratype area.
6. Suturing the incisions and, after assessing the width of the nostrils, if necessary, partial resection of the wings of the nose can be performed (Weer operation). After obtaining a satisfactory aesthetic result of the patient's profile, all incisions are sutured with 5.0 catgut. To correct the width of the nostrils, partial resection of the wings of the nose is performed by excision of the skin and soft tissues from their base with a 6.0 Prolene or 6.0 Monocryl suture.
7. Narrowing of the nasal dorsum using lateral osteotomy.
Through separate incisions-punctures in the vestibule of the nose at the base of the pyriform opening, a lateral osteotomy is performed (it is desirable that the osteotomy line is clean and as low as possible) with osteotomes with the right and left curvature to the inner corners of the eyes, followed by infracture (inward fracture) and wedging of bone fragments in new position. Lateral osteotomy is performed on both sides to achieve mobility of the nasal bones, and then to reposition them (new position) to bring them closer together.
8. Insertion of turundas into the nasal passages and application of a multilayer bandage made of plaster and plaster.
Turundas introduced after rhinoplasty (gauze strips soaked in a special oil that prevents drying, which is especially important when they are removed the next day) exert mechanical pressure on the vessels and are placed to prevent nosebleeds in the early postoperative period. And they also help the surgeon put on an aesthetically correct plaster cast, pressing from the inside.
Open and closed (endonasal) approaches in rhinoplasty
External approaches, when considered in a historical context, have gone through more than two centuries from skin grafting from one of the arms (the arm was “fixed” to the head with a bandage, and the patient had to wait until the skin took root) to “virtually invisible” seagulls" (most often the external access is located in the lower part of the columella and is shaped like a gull's wing). External incisions have one very significant advantage: they allow the surgeon to widely expose almost all structures of the nose and work with them ad visum (under visual control). Disadvantages: contraction of the subcutaneous scar is not always predictable (it often looks retracted and deforms the collumela), more pronounced swelling in the postoperative period (most likely due to greater trauma to the vessels supplying the tip of the nose), and most importantly, it is noticeable! External approaches have a right to exist and are advisable for severe post-traumatic (or when it is impossible to perform endonasal approaches, for example, after thermal damage to facial tissues) deformities of the nose. Internal approaches are used in rhinoplasty to correct all parts of the nose. We have already mentioned them, but let's try to understand them again:
1. Transfection approach - passes between the lower edge of the septal cartilage and the upper edge of the medial crura of the alar cartilages. It is used to shorten and rotate the tip of the nose with resection of the distal part of the septal cartilage and to shorten the collumella when it is sagging.
2. Regional access (also called anterior endonasal) - located almost immediately behind the edge of the nostril (2-3 mm) and along it. It is needed for isolating the alar cartilages and working with them (most often used to narrow the tip of the nose in the front and lower the projection of the tip of the nose; many surgeons also use it to “exit” to the dorsum of the nose, avoiding intercartilaginous and transcartilaginous approaches).
3. Transcartilaginous (middle endonal) and intercartilaginous (posterior endonal) approaches are carried out in the middle or along the upper edge of the lateral crura of the wing cartilages. They make it easy to correct both the cartilaginous and bony parts of the dorsum of the nose, as well as after the so-called. “luxation” to perform the necessary manipulations with the wing cartilages.
Rehabilitation
The plaster cast is worn for 7-10 days. It helps control post-operative swelling and also keeps the nasal bones in their new position and prevents them from moving apart. Cold (most often ice or special glasses) must be used in such a way that it does not dissolve the plaster cast (by direct contact of water with the plaster), so use it separately on the right and left. It makes sense to do this 3-4 days after rhinoplasty for 10-15 minutes 3-4 times a day. Usually our patients receive a special postoperative kit, which includes any of the kernel oils - peach or almond, apricot (oil solutions lubricate the nasal mucosa well, facilitate the separation of crusts, which form especially intensively in dry air conditions, so it is recommended to humidify the air in which the patient is located using humidifiers or simply by placing a container of water on low heat, adding a couple of drops of eucalyptus tincture) and a rinsing solution, for example, aquamaris. Do not try to remove the “thread knots” lovingly tied by surgeons and do not cut them yourself - this can lead to suture divergence and then to severe scarring! Physiotherapeutic procedures are needed to reduce the rehabilitation period by additionally influencing the rate of resolution of postoperative edema, but you need to know about them Cosmetologists-rehabilitologists can tell you better.
Conclusion
Rhinoplasty is by far one of the most favorite operations for both surgeons and patients, reminding me of an ocean liner where once you get on board you know that you will have to sail for a long time