The mammary glands, the main symbol of femininity, begin to develop already in utero, and reach their maximum development during lactation.
Congenital malformations of the mammary glands occur in 2–6% of women, their severity varies from relatively minor to major deformities of the mammary glands. Minor malformations may not even be recognized, while severe deformities can cause significant functional, psychological and aesthetic problems.
Changes in shape can be due to excessive (hypertrophy) or insufficient volume (atrophy, hypotrophy) of the mammary glands, uneven development (asymmetry) or malformations (tubular deformation). Tubular deformation of the mammary glands can affect a woman's ability to breastfeed.
Breast shape is affected by:
- Volume of breast parenchyma
- Amount and location of subcutaneous and intraparenchymal fat
- Anatomy of the chest
- The muscular frame in the thoracic region, the degree of its development
- Skin elasticity
The fascial attachments of the mammary glands also affect the appearance of the breasts. The mammary glands develop between two layers of superficial fascia. The superficial layer of the superficial fascia, located near the dermis and not always different from it, covers the parenchyma of the mammary gland. More distinct is the deep layer of superficial fascia located on the posterior surface of the breast. The free areolar region is located between the deep layer of superficial fascia and the superficial layer of deep fascia, which covers the outer layer of the pectoralis major muscle.
Tubular breasts have several variations, and to correct each of them, the plastic surgeon must know all of these variations. Having correctly determined the type of tubular breast, the doctor can competently plan and perform the operation itself.
Reasons for the formation of tubular breasts
To date, there is no consensus among scientists about the causes of the formation of tubular breasts.
It is only considered proven that the formation of tubes is due to a genetic predisposition, so a woman often receives such breasts “inherited”. According to one theory, tubular breasts occur due to improper development of the fascia (the connective tissue membrane that covers all our organs) - its high degree of rigidity.
As a result, during the period of growth, the breast cannot acquire an anatomically correct hemispherical shape; it grows only towards the nipple, the areola stretches, and a hernia forms around it. According to another version, the reason lies in the overly dense consistency of the mammary gland, which again prevents the breast from acquiring the shape of a hemisphere.
Anatomy and embryology of the mammary glands
Embryologically, the breast is formed from the mammary ridge, which develops in utero from the ectoderm, starting from the 5th week of pregnancy. Soon after its formation (7–8 weeks), most of this ridge disappears, with the exception of a small part in the thoracic region, which persists and penetrates into the underlying mesenchyme (10–14 weeks). Further differentiation and development of the mammary gland occurs during intrauterine life and is completed by the time of birth, after which essentially no further development occurs until puberty.
The next stage of breast development begins during puberty and is characterized by the growth of breast tissue. At this time, the breasts take on their usual shape.
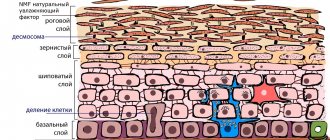
As a result of the ectodermal origin of the mammary gland and its invagination into the underlying mesenchyme, the mammary gland tissue is “wrapped” in a fascial sheath (superficial fascia).
This superficial fascia is a continuation of the superficial abdominal fascia and consists of two layers: the superficial layer of the superficial fascia, which is the outer layer covering the parenchyma of the mammary gland, and the deep layer of superficial fascia, which forms the posterior border of the mammary parenchyma and lies on the deep fascia of the pectoralis major and serratus anterior muscles.
The deep layer of superficial fascia is pierced by fibrous bridges called Cooper's ligaments, connecting the two layers of superficial fascia and extending to the dermis of the overlying skin and deep pectoral fascia.
A critical point in understanding tubular breast deformity is the fact that the superficial layer of superficial fascia is absent in the area under the areola.
Clinical experience has shown that in cases of tubular breast deformity, there is a tapering fibrous ring at the level of the periphery of the nipple-areolar complex, which prevents the normal development of the mammary gland.
This tapering fibrous ring is denser in the lower part of the breast and prevents the developing breast parenchyma from expanding during puberty. It represents a thickening of the superficial fascia.
The result of this is that the developing breast cannot expand, and since there is no superficial layer of superficial fascia beneath the areola, the breast parenchyma forms a hernial protrusion towards the nipple-areolar complex.
The severity of the deformity depends on the severity of the deformation of the superficial fascia and varies from slight underdevelopment of the lower medial quadrant of the breast with almost normal breast volume to significant hypoplasia in all four quadrants of varying degrees.
Degrees of manifestation of breast tubularity
It is customary to distinguish three degrees of tubular breast severity:
1. Type I tubularity is characterized by a slight deficiency of breast tissue inside and below the breast. The breast is slightly raised up, and the nipple, on the contrary, is lowered.
2. Type II tubularity is characterized by a lack of glandular tissue along the entire lower slope of the chest and in its lateral sections. The breast is already noticeably moving downwards, the nipple looks flat, and the areolas take up more space.
3. Type III tubularity indicator - a serious deficiency of glandular tissue over the entire area of the chest. The mammary gland is greatly elongated, the areola is stretched, and the nipple becomes completely flat.
A woman does not always know that she is a carrier of tubular breasts. Often, such patients turn to a plastic surgeon to enlarge the mammary glands or do a breast lift, mistaking tubularity for ptosis. In fact, surgery to correct tubular breasts is much more complicated than classic augmentation mammoplasty or breast lift. The surgeon’s task is to identify the degree of breast tubularity and correctly plan the operation so as not to get such a common complication as a “double bubble” - the formation of a fold along the lower slope of the mammary gland.
Complications that occur after surgery
Upon completion of surgery, patients are faced not only with complications provided for by the procedure.
A frequent complaint is a decrease in the sensitivity threshold of the breast. Sometimes such a problem turns from temporary to permanent.
Quite rarely, complications appear as hematomas and purulent formations. Such negative consequences are caused by the poor quality of the surgical procedure and the inadequate qualifications of the plastic surgeon.
Among individually expressed complications, keloid scars are considered the most common.
To mitigate unforeseen complications, you must carefully select a plastic surgeon.
Correction methods
To correct tubular breasts, as a rule, they resort to complex mammoplasty, which may include endoprosthetics, lifting and flattening, and the formation of a glandular flap according to Botti, the author of this technique. In some situations, lipomodeling may be sufficient, provided that the tubularity is mild and the surgeon does not face other aesthetic problems. In general, surgery to correct tubularity is reconstructive in nature and requires a high level of professionalism and skill from the doctor.
Step by step execution of the operation
When diagnosed with tubular breast, surgical intervention is of a reconstructive nature. It involves reducing the size of the areolas while simultaneously changing the shape of the mammary glands.
During the consultation, the plastic surgeon recommends that the patient reduce, or better yet eliminate, alcohol consumption, smoking, and taking medications that affect blood clotting.
The step-by-step implementation of plastic surgery includes a set of measures.
- After general anesthesia, 2 incisions of a fixed diameter are made on the areola.
- Next, the size of the area around the nipples decreases.
- A cavity is then created, referred to as a “pocket”.
- Next, preparations are made for the insertion of silicone implants.
- Then the doctor inserts a tube with a vacuum into the chest area to subsequently remove the formed blood clots from the mammary gland.
- At the end of the event, the specialist sews the fabrics and cut edges together.
The effect of the operation is visible after (approximately) 6 months.
A positive aspect of such an event is the preserved possibility of breastfeeding, which is important for women planning to have children.
Features of tubular breast surgery
The operation process consists of several main stages. At the first stage, the doctor works on the size of the areolas - makes diametrical incisions and removes excess skin around them. Next, having reduced the size of the areolas, the surgeon dissects the mammary gland in several places to make its base wider and correct tubular deformation. At the third stage, the surgeon gives the mammary gland a flat, spread-out shape and forms a pocket for the implant. At the last stage of the operation, the doctor evenly distributes the breast tissue over the surface of the implant and applies sutures.
In some cases, tubular breast correction cannot be performed in one operation. The installation of implants may be preceded by expanders - special hollow prostheses that are filled with saline solution in order to stretch the tissue. After a few weeks, the expanders are removed and replaced with implants of the required size.
The surgical plan is discussed individually by the plastic surgeon and the patient during a face-to-face consultation.
Tubularity is a form in which the breast does not look like a hemisphere, but like an elongated tube. The nipples and areolas are usually enlarged. The reasons for the development of tubular breast form are genetic. The fascia (a sheath of connective tissue) may be too stiff and prevent the gland from spreading evenly and forming a hemisphere shape. Or the gland itself may be too dense, which also makes it difficult to form a hemispherical shape. The chest begins to grow forward and stretches into a tube.
Tubular breast shape
Tubularity is also characterized by:
— hypoplasia (underdevelopment) of the breast;
- incorrect (high) position of the inframammary fold;
- areolar hernias;
- the areola and nipple are usually enlarged and located in the lower part of the gland;
- significant space between the glands;
- breast asymmetry.
A woman may have one, several, or all of these anatomical signs—tubularity may occur to varying degrees. From almost invisible, when the glands are slightly directed upward and the nipple is slightly directed downward. Up to the mammary gland in the form of a “mushroom”, when the base of the gland is not large enough, and improperly developed areolas with an areolar hernia exceed it in size and therefore resemble a mushroom cap.
Tubular deformation is common. It is not harmful to health and in most cases does not affect breastfeeding, but it can significantly affect self-esteem.
Features of tubular breast enlargement
The tubular form complicates breast augmentation surgery. The tubular shape cannot be corrected only by increasing implants:
1) Sufficiently dense fascia with tubularity does not allow the gland to expand on the implant.
2) The tubular breast has almost no lower pole (it is very short) and if you simply install an implant, the nipple will slope down unsightly.
Therefore, a complex of manipulations is necessary.
1) Dissection and spreading of the gland and fascia. The fascia of the gland is cut in several places to straighten it and increase its area. The gland is then cut and the breast tissue is redistributed.
In order for the breasts to acquire a rounded shape, you need to lower the inframammary fold.
2) It is advisable to supplement the shape correction with lipofilling. By adding auto fat, you can fill the lower pole of the breast.
Lipofilling will not dramatically increase breast size (by 0.5-1 size, rarely by 1.5 sizes). Therefore, if the patient’s goal is a greater increase, and the anatomy allows this, lipofilling can be combined with the installation of implants.
If the tubular breast is initially large and requires a lift, a lift can be done using implants with a lowering of the inframammary fold. In this case, lipofilling may not be necessary.
If the anatomy allows you to obtain the result in one stage, the surgeon will offer a combined operation - installation of implants in combination with lipofilling. If this is not possible, the surgeon will suggest a correction in two stages: first, lipofilling and after 4 months, when the tissues have stretched and changed configuration, the surgeon installs implants.
Access Features
All approaches can be used depending on the patient’s initial data. If tubularity is pronounced, access along the lower edge of the areola is mainly used.
I choose the submammary approach when it is necessary to lower the submammary fold. It is not advisable to do this through the areola, since the new submammary fold must be fixed so that the implant does not move lower.
If the patient wants the nipple to be higher, it must be transferred. The decision on the method is made individually. It depends, among other things, on the chosen implant.
If a lift is necessary, an incision is made around the areola, vertically and along the inframammary fold. Thanks to the T-lift, fabrics can be cut, redistributed and folded in the best possible way to achieve the most beautiful shape. In addition, tissue tension after surgery will be applied to three scars. The load on each of the scars will not be so great, so there is a chance to keep the scars thin.
Other types of incisions when lifting tubular breasts limit the quality of the result, since neither through the areola nor with a vertical lift it is possible to work with the lower pole.
If there is ptosis and tubularity, and the patient does not want additional scars (except on the areola), the surgeon will talk about the risks and possible complications - the possibility of scar divergence, obtaining a specific shape of the breast and areola.
Rehabilitation and feeding options
Surgery to correct tubular breasts is more traumatic, since the surgeon also dissects the gland (with conventional breast augmentation, the gland is usually not affected). However, this has virtually no effect on the speed of rehabilitation, the duration and volume of swelling and bruising.
It is worth noting that if the ducts are not damaged during work with the gland, the patient can continue to breastfeed. If the duct gets into the scarring area, then most likely, feeding will no longer be possible.
To communicate with patients who have undergone breast augmentation, lifting or reduction, come to our forum in the Mammoplasty
This is not a public offer. There are contraindications. Before use, consultation with a specialist is required.
Stages of surgery to correct tubular mammary gland
Correction of tubularity is considered to be one of the most difficult manipulations among breast correction operations. The procedure requires a specialist to have a lot of experience and an intuitive understanding of the problem. This is due to the fact that each anomaly is unique and requires an individual approach.
The surgical adjustment process consists of four stages:
- Changing the existing breast shape.
- Mammoplasty of the tubular mammary gland by introducing a silicone implant.
- Correction and movement of the areolar area to a higher point.
- Formation of the correct inframammary fold.
A mandatory element of a high-quality operation is the elimination of the periolar hernia (if any) and the correction of the asymmetry of the glands.
If there is a large deficiency of soft tissue, additional intervention may be required: first, an expander is introduced to help stretch the fibrous fibers, and then an endoprosthesis is placed.
Selection of implant
Tubular breasts can be corrected using both anatomical and round implants. The shape of the prosthesis depends on the individual body proportions and other characteristics of the patient.
Anatomical implants are suitable for girls who want to get the most natural breast shape with smooth contours and curves. Ideal for fine-boned ladies with elastic skin.
Round endoprostheses give a slightly “doll-like” volume by filling the upper section and creating a raised bust. Such implants are recommended for girls with a sufficient amount of their own tissue.
Plastic surgeons advise choosing prostheses based on the width of the chest and the base of the mammary gland. It is better to listen to the recommendations of a specialist who, due to knowledge and experience, is well versed in all the intricacies of choosing and installing an implant.
Prosthetics
The endoprosthesis is inserted in two projections: the upper part is placed under the pectoralis major muscle, and the lower part is placed under the mammary gland. To do this, the specialist makes an incision along the boundaries of the areola and breast tissue. The skin flaps are turned away, the cords that interfere with the growth of the gland are excised. An implant is inserted into the resulting space.
After installing the endoprosthesis in place, the remaining blood is sucked out, the internal tissues are stretched and stitched, and cosmetic sutures are applied to the surface.
If the breast is very small and the skin is poorly stretchable, an expander is installed in the cavity obtained after excision, which is regularly pumped with solution. This allows you to gradually and painlessly increase the volume of the mammary gland. The stretching process takes 6–8 months.
Breast lift (mastopexy)
To get rid of defects in the nipple-areolar area, the mastopexy method is used. The manipulation involves removing excess skin, eliminating breast ptosis and nipple displacement. This type of lift is recommended for women with any degree of anomaly. It is performed simultaneously with mammoplasty.
Features of the tubular bust
Often, only one mammary gland is subject to deformation. The volume of the bust itself can be either large or small. The cause of the defect is the improper development of connective tissue and ligamentous apparatus, which is genetically determined and inherited. The pathology cannot be called rare - according to statistics, there is 1 case in 40-50 women.
In addition to the obvious, visually noticeable defect, there is also a hidden one, which is more difficult to diagnose. Often underdeveloped ligaments are detected on the operating table.
Rehabilitation
After the operation, the woman remains in the clinic for a day under the supervision of doctors. To reduce pain, special painkillers are prescribed. The next day after surgical procedures, the surgeon performs the first dressing. The first days you should sleep on your back, and remove the bandage only a week after the plastic surgery.
Upon discharge, the surgeon gives the patient a sheet of recommendations that must be strictly followed during the rehabilitation period. After surgical treatment it is necessary:
- refuse heavy physical activity;
- visit the clinic for dressing changes;
- for six months do not visit the bathhouse or sauna, do not take a hot bath;
- Avoid exposure to direct sunlight, avoid solariums;
- wear compression garments (1-2 months);
- perform light exercise to improve wound healing (prescribed by your doctor).
After the operation, normal activity begins already on the 3rd day. 2 weeks after plastic surgery, a woman can return to everyday life.
Among the special medical recommendations: ultrasound of the mammary glands - annually, follow-up examinations with a doctor - at 3.6 weeks, 3, 6 and 12 months after surgery.