After surgery, in some cases, a complication such as seroma occurs. So what is it? This is an accumulation of serous fluid in the area of the surgical wound. Seroma occurs especially often in obese people. When such a disease develops, a serous, odorless, straw-colored fluid begins to leak from the wound; the disease is accompanied by severe swelling and, in some cases, pain.
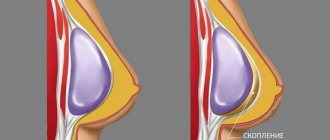
Quite often, seroma occurs after various plastic surgeries . In many cases, it can resolve on its own in about two weeks. At the same time, a large amount of seroma leads to stretching of the skin, as a result of which it begins to sag unsightly. All this causes great anxiety and discomfort in the patient. This complication leads to an increase in the recovery period and regular visits to the doctor. The photo clearly demonstrates what a seroma looks like.
What is seroma
Seroma is a disruption of the natural healing of the epithelial surface and soft tissue in the area where surgical procedures were performed. In the subcutaneous space between the fat layer and the epithelium, a straw-colored liquid begins to form, which does not have a pronounced or other specific odor.
The main localization of seroma accumulation is the intersection of the smallest capillary vessels.
The basis of the serous fluid is lymph, which begins to collect due to the prolonged absence of the wound healing process, or cell division occurs too slowly.
In 85% of cases, seroma is not an independent disease, but acts as a symptom that signals the presence of concomitant pathology that disrupts the normal recovery of the body after surgery. The appearance of lymphatic accumulations at the site of a surgical scar is a reason for a more detailed examination of the body.
Causes of seroma formation
Seroma of a postoperative suture is a pathological condition of the subcutaneous surface and circumference of soft tissues that does not occur independently without the negative influence of one or several factors at once. In the vast majority of clinical cases, the appearance of an excess amount of serous fluid in the area of the postoperative scar occurs for various reasons.
They are as follows:
- excessive activity of the lymphatic system, which reacted too sharply to mechanical damage to the skin, causing a local inflammatory process with an abnormally large release of lymph;
- the presence of elevated blood sugar levels, which is caused by concomitant diabetes or impaired body tolerance to glucose molecules;
- excess body weight, characterized by a thick layer of fat in the area of the body in which surgery took place;
- reaching 75 years of age or older (patients in this age category do not tolerate surgery well, and postoperative rehabilitation is even worse, since due to physiological changes, cells are no longer capable of rapid division);
- hypertension, when due to an increased level of blood pressure, an uneven redistribution of lymphatic fluid throughout the body occurs and it begins to accumulate in the area of damaged tissue.
Depending on the individual characteristics of the patient’s body, hereditary factors, lifestyle, quality of nutrition, the presence or absence of bad habits, there may be the influence of other reasons that can also slow down the healing process of the surgical suture and serve as a prerequisite for the formation of seroma.
Causes and treatment of seroma after abdominoplasty
Abdominoplasty is included in the category of the most complex plastic surgeries. Surgical tummy tuck traumatizes an impressive area of skin and deeper structures, for example, the muscular aponeurotic layer. The risk of occurrence is quite large, and it becomes even higher if the patient has certain diseases, medical errors and non-compliance with the rules of the rehabilitation period.
Negative consequences include seroma after tummy tuck. Seroma refers to the accumulation of lymph fluid between tissues that were involved (injured) during surgery. According to statistics, such a complication forms in the suture area, i.e. future scar. Lymph collects in the cavity between the fat layer and injured capillaries, and can accumulate there for several weeks and months.
In what case is seroma considered a serious complication and what reasons can cause its appearance? When should a patient be wary and seek medical help in time? Is it possible to prevent the development of seroma?
Why does seroma appear after a tummy tuck?
During abdominoplasty, no matter how carefully the surgeon acts, he cannot avoid rupturing or cutting the lymphatic vessels. While blood vessels can quickly close with a thrombus, lymphatic vessels do not have this feature, so even after suturing, fluid (exudate) leaks out of them. Since the correction area is large and the incision is located in the pubic area, the patient is unable to create rest conditions for the injured tissues. Movement and sometimes even breathing can promote tissue movement, which again causes fluid to be released. In cases where the outflow of this excess fluid does not occur quickly, a seroma appears. Typically, the following factors increase the risk of developing seroma:
- Severe tissue damage. Normally, a plastic surgeon carefully and scrupulously separates healthy and pathological tissues. But if the doctor works clumsily and sloppily, he thereby increases the risk of free cavities appearing in the area of the future scar, where exudate will drain (be released).
- Increased immune activity. Lymph contains leukocytes, which perform a protective function in the body. In some cases, lymphatic fluid is formed in a larger volume and increases the likelihood of seroma formation. A long inflammatory process in the scar area leads to the same result. The longer the suture takes to heal, the higher the risk of seroma.
- Cardiovascular diseases . Fluctuations in blood pressure, disturbances in blood lipid balance and vasomotor reactions - all this contributes to the negative development of events.
- Increased body weight . It is generally accepted that if there is subcutaneous fat thicker than 5 cm, seroma will certainly occur.
- Elderly age. In people over 70 years of age, regeneration processes are much slower than in representatives of the younger generation. It is understandable why this category of patients will have a higher risk of seroma.
Signs of seroma
Seroma usually forms within 1-2 weeks after abdominoplasty. Its volume can be either small - from 10-20 ml, or quite impressive - up to 1-2 liters. It is quite difficult to understand that it is a seroma when it is small in size, since there are no pronounced symptoms. But when the volume of seroma reaches 0.5 liters, it is unlikely that seroma will be confused with something else.
At this stage, local swelling and discomfort appear in the scar area - aching or nagging pain. The patient may feel a “transfusion” of fluid in the problem area, notice hyperemia in the area of the body where serous fluid has accumulated. Many patients have a fever (37-37.5 degrees).
There is general weakness and fatigue. The listed signs are usually noticed by the patient himself. After contacting a plastic surgeon, other symptoms become known and are diagnosed by the doctor. The doctor notes an increase in the size of the abdomen, fluctuation and local hyperthermia.
Additionally, it is necessary to perform hardware tests. In these cases, the doctor prescribes an ultrasound, during which it will be possible to distinguish healthy tissues and cavities filled with lymph on the monitor. The doctor should also take a puncture to eliminate the risk of an abscess.
Will seroma resolve on its own?
In many cases, seroma resolves on its own, but even in this situation, the plastic surgeon carefully monitors the process, since at the slightest deviation from the norm, seroma can cause more serious negative consequences. Among them:
- Seroma suppuration. An extreme case is an abscess (purulent inflammation of tissues with their melting and the formation of a purulent cavity).
- An increase in cells that produce mucous fluid, which prevents the walls of the serous “pocket” from growing together. These circumstances aggravate the situation and complicate treatment.
- Deformation of the abdominal wall, thinning of the subcutaneous fat, the appearance of excess scar tissue. All of these signs are not dangerous to health, but they worsen the aesthetic appearance of the abdomen.
At a face-to-face consultation with Dr. Svetlana Pshonkina, find out how to avoid gray
How to treat gray
After abdominoplasty, drainage tubes are required to remove biological fluids from the body. The drainage system is removed after the volume of fluid does not exceed 20-30 ml per day. According to medical calculations, such an amount of exudate should not become a problem for the body, which must independently cope with the processing of this volume of liquid. This usually takes the body 2-3 weeks.
If the seroma only increases in size, the patient’s condition worsens, or the wound becomes infected, the doctor prescribes antibacterial drugs. Medicines should improve the outflow of lymph, reduce the cavity of accumulation of serous fluid, and eliminate the development of infection. In addition, the patient is prescribed drugs from the group of non-steroidal anti-inflammatory drugs (Diprospan and Kenalog).
If the treatment described above does not bring benefit, the doctor performs vacuum aspiration of the seroma. This is a surgical procedure during which the doctor makes an incision in the area of fluid accumulation. Through this incision, a special tube is installed inside, through which the serous contents are suctioned. In most cases, after the procedure there is significant relief and improvement in the condition, however, in non-acute patients, due to the individual characteristics of the body, a relapse may occur and aspiration will be required again.
Prevention of seroma after abdominoplasty
It is possible to prevent the occurrence of such a complication, but not only the surgeon, but also the patient himself must work well here. As for the surgeon, the specialist, even at the stage of planning the operation, must assess the risk of seroma and, if necessary, give certain recommendations to the patient. Directly during abdominoplasty, the doctor must work with the tissues extremely carefully and also carefully apply sutures to the wound in layers. After the operation, the surgeon installs a drainage system and prescribes the patient a course of antibiotics.
For his part, the patient must reach a comfortable weight and get rid of extra pounds. After a tummy tuck, you must wear compression garments and avoid physical activity, bending over, and lifting heavy objects. Do not skip examinations with a plastic surgeon.
According to plastic surgeons, it is not worth calling gray a complication, since this phenomenon represents only the specifics of the functioning of the body’s lymphatic system in a particular patient. But do not forget that if you have any disturbing pain symptoms, you should immediately consult a doctor, and not hope and wait for the problem to be solved on its own.
Make an appointment with Svetlana Pshonkina for a free 40-minute consultation on abdominoplasty +7 (495) 773-04-54
Symptoms
Suture seroma, which appears during postoperative recovery of the body, is always a local inflammatory process, characterized by the occurrence of concomitant signs of the disease.
They are:
- an increase in body temperature, which reaches 37-39 degrees and directly depends on the level of the human immune system, the presence of infectious agents, and the extent of inflammation;
- a feeling of aching pain that may not stop for several hours, subside for a while, and then resume again;
- swelling of the soft tissues and epithelial surface located around the postoperative suture, which is the first sign of abundant accumulation of seroma between the lipid and dermal layers;
- burning pain syndrome that occurs when the surgical area is inclined and there is an influx of additional blood and lymph;
- redness of the skin around the postoperative suture, the color of which depends on the severity of the inflammatory process and can vary from pale pink to deep purple and bluish.
The main symptom of the formation of a seroma can be considered the release of lymphatic fluid, which protrudes directly between the edges of a wound that has not yet healed.
If the complication occurs without worsening the clinical picture, then upon examination a yellowish-tinged liquid without a foul odor is observed, and its appearance always indicates the addition of a fungal or bacterial infection.
Symptoms of seroma
Seroma can be suspected if the following symptoms are present:
- The patient feels as if fluid is beginning to overflow in the lower abdomen.
- Sometimes there is swelling and a feeling of bulging in the lower abdomen. Patients claim that their abdomen has suddenly increased in volume, although this was not the case a few days ago.
If the serous fluid has reached large volumes , then the following symptoms occur:
- Soreness or a feeling of tension in the area where the seroma has accumulated. Most often this is the lower abdomen.
- Nagging pain that begins to intensify if the patient gets to his feet.
- Redness of the skin in the place where the seroma has accumulated the most.
- General weakness, increased body temperature up to 37 degrees, fatigue.
Treatment of seroma
This disease is treated in two ways:
- surgical method;
- by medicinal method.
For surgical treatment, puncture is used. This is the most common method used to remove fluid. In 90% of cases this brings a positive result. Using a syringe, the surgeon removes serous fluid, the volume of which can reach 500–600 ml. Seroma should be pumped out constantly , every 2 - 3 days. To completely get rid of it, 3 to 7 punctures are performed. In particularly severe cases, more than 15 punctures may be required. After such manipulations, the amount of serous fluid decreases.
In patients with a large thickness of subcutaneous fat, the seroma is large and therefore puncture is usually not enough. Therefore, it is necessary to install drainage with active aspiration . The fluid begins to constantly drain through the drainage, decreasing in volume, and after some time the cavity will close, grow together and the seroma will disappear.
The medicinal method of treatment consists of using:
- antibiotics with a broad spectrum of action;
- non-steroidal anti-inflammatory drugs, which are used to relieve aseptic inflammation and reduce the amount of fluid;
- Sometimes steroidal anti-inflammatory drugs such as kenagol and diprospan are prescribed, which relieve inflammation well and reduce the amount of fluid.
Prevention of seroma formation
Preventive measures are based on compliance with the following surgical principles:
- You should not do abdominoplasty if the thickness of the subcutaneous fat of the anterior abdominal wall is more than 5 cm. First, you need to remove unwanted fat deposits and only after 3 months you need to plan abdominoplasty.
- Soft tissues should be handled with care . Electrocoagulation must be used in isolation, cauterizing only bleeding vessels.
- It is necessary to maintain physical rest in the first weeks after surgery . This is necessary so that the movement of the soft tissues of the anterior abdominal wall relative to each other is significantly reduced.
Thus, seroma is a rather unpleasant complication and under no circumstances should you ignore it. This disease will not go away on its own and must be treated.
Only timely, competent treatment can guarantee excellent results and complete recovery.
Diagnostics
Postoperative suture seroma is a disruption of the natural wound healing process, the appearance of which requires not only local treatment, but also a comprehensive diagnosis of internal organs and systems in order to eliminate the cause that impedes normal recovery.
To do this, the patient is prescribed the following diagnostic procedures:
- collection of serous fluid to exclude infection;
- donation of capillary blood from a finger for clinical analysis of glucose levels, as well as the percentage of platelets, erythrocytes, phagocytes, lymphocytes;
- venous blood for its biochemical diagnosis for cancer cells, strains of pathogenic microorganisms (tuberculosis, syphilis, HIV);
- swab from the surface of the seam.
In case of urgent need and suspicion of an inflammatory process occurring in the soft tissues of the surgical site, ultrasound diagnostics can be used. Based on the results of the examination, a decision is made on the formation of a course of therapy.
Possible complications
By its nature of origin, the accumulation of serous fluid under the skin surface of the postoperative suture is already a complication of the normal wound healing process.
If no therapeutic measures are taken, the following pathologies may develop:
- formation of deep scars and keloids;
- penetration of a bacterial infection into the gray;
- rotting of the postoperative suture;
- extensive inflammation spreading to the surrounding tissues, and in some cases even internal organs;
- the appearance of fistulous holes, from which purulent contents are periodically released.
The most severe complication of seroma of the postoperative suture is blood poisoning, which leads to the onset of septic shock and ends in death. This scenario is possible in advanced forms of the disease.
Why does it appear after surgery?
During surgery, natural damage to cells and various blood vessels (including capillaries) occurs.
As a result, fluid accumulation may begin in the tissues between the dermis and subcutaneous fat. Serous matter is essentially lymph; it contains formed elements of blood, as well as a certain amount of protein fractions. As a rule, such a liquid has a straw color, but occasionally it can be reddish (if there is a significant number of leukocytes in the composition).
The accumulation of serous fluid after surgery does not always pose a threat to human health. However, seroma can cause sagging skin at the site of the intervention and also complicate the healing process.
At-risk groups
The likelihood of seroma occurring is especially high if:
- Sloppy work of the surgeon. If the doctor performs a series of not very careful actions, he can harm the surrounding tissues. Such injuries provoke the release of lymph.
- Inflammatory process. Sometimes it is only a consequence of tissue damage and is non-infectious in nature. But increased formation of serous fluid is characteristic.
- Hypertension. When blood pressure increases, the full distribution of lymph in the body is disrupted, which can lead to its sweating through capillaries damaged during the intervention.
- Excess body weight. Seroma is diagnosed after surgery in approximately 75% of obese patients.
- Diabetes mellitus. This disease is characterized by an increase in blood glucose. Due to its excessive amount, it is difficult for the body to recover after surgery, the process of tissue regeneration slows down (including the restoration of blood vessels).
- Old age. Over the years, metabolism naturally slows down, which is why the rate of regeneration also decreases. The risk of serous fluid formation increases.
- Soft tissue burn. If the surgeon does not use the electrocoagulator carefully enough when cauterizing injured vessels, a small focus of necrosis may appear in the affected area, in which, in turn, serous fluid will accumulate.
A particularly high risk of developing postoperative suture seroma is observed during interventions on the abdominal cavity, as well as on the mammary glands.
Typically, doctors take all possible measures to reduce the likelihood of such a complication.
Due to caesarean section
Seroma of the postoperative suture in women who gave birth to a child through surgery is a fairly common complication. The most common reason is a weakened body caused by a long pregnancy, due to which the regeneration processes slow down by an order of magnitude.
Seroma after cesarean section has a fairly typical appearance - a small, dense ball filled with exudate (lymph) appears on the suture. The appearance of such a disorder is associated with damage to blood vessels as a result of the incision.
Most often, seroma of the postoperative suture, resulting from a cesarean section, does not cause any discomfort to the mother in labor and does not require treatment. But in any case, it is imperative to inform doctors about its appearance.
Postoperative suture seroma after cesarean section
After the birth of a child through surgery, the appearance of signs of accumulation of serous fluid cannot be ruled out due to the large size of the suture and the extensiveness of the wound surface.
In this case, the mechanism and features of the development of pathology are as follows:
- immediately after the completion of labor, the abdomen still retains large volumes, so the edges of the wound do not fit tightly;
- on this basis, a sluggish inflammatory process occurs;
- the woman’s body is in a weakened state, which affects the protective function of the immune system, which cannot fully ensure rapid healing of the suture;
- swelling and inflammation of the surrounding tissues continues to increase, which ultimately leads to the accumulation of serous fluid, the volume of which directly depends on the severity of the current pathology.
Experienced surgeons, obstetricians and gynecologists promptly introduce corrective actions into the therapeutic process to avoid the development of postoperative complications of cesarean section.
Seroma formation after mastectomy and abdominoplasty
At least 15% of clinical cases of abdominoplasty and mastectomy result in the formation of serous contents. The peculiarities of the formation of seroma after operations of this type are associated with the fact that the mammary gland in women mainly consists of adipose tissue and lymph nodes.
The mastectomy procedure itself and plastic surgery involve large incisions, as a result of which elements of the lymphatic system are damaged.
In this case, the accumulation of serous fluid is a protective reaction of the body.
The mechanism of seroma formation is similar; it occurs due to the direction of additional fluid volume by the lymphatic system. As anti-inflammatory and other therapeutic measures are carried out, the swelling subsides, and the excess amount of serous fluid is removed outside the body.
Possible complications after abdominoplasty
The purpose of this literature review is to systematically present the available data on the incidence, prevention, and treatment of the most common complications after abdominoplasty. Although, it would be desirable to conduct a more comprehensive methodological analysis of the articles mentioned in this review. This would help focus on specific aspects of abdominoplasty complications rather than a comprehensive review. For this reason, the authors limited themselves to mentioning the design of each study, as well as the corresponding level of evidence for the studies cited in this article. A statistical meta-analysis of the findings was beyond the scope of this study, mainly due to the heterogeneity of the studies reviewed.
Another limitation worth mentioning is the fact that 9 of the 119 studies were excluded because they were published in languages that were not understood by the authors. The remaining 110 articles were in English, and only 1 article was published in Spanish. Ideally, a future review would not include language as part of the inclusion criteria. For the same reason, it would be interesting to include other indexing databases in a systematic search strategy, especially those containing unpublished results. This is especially true as there may be complications in the scientific literature that may lead to underestimation.
As presented in the Results section, abdominoplasty, with or without liposuction, is a safe procedure when adequate precautions are taken before, during, and after surgery. Patient preparation is of utmost importance. It is during the initial consultation that the problem of quitting smoking can be addressed, potentially reducing the risk of infection and skin necrosis. Similarly, it is possible to diagnose and treat patients suffering from iron deficiency anemia. Up to 10% of women of childbearing age have hemoglobin concentrations below 12 g/dL.
During the operation, high-quality surgical technique is necessary, based on the latest data and the individual experience of the surgeon. The search for improved aesthetic results and reduced complication rates should motivate each practitioner to hone their abilities and make adjustments as necessary. Over the past decades, it has been proven that the addition of liposuction to abdominoplasty does not expose patients to additional risk as long as flap perfusion is ensured by maintaining a sufficient number of perforators during dissection. With regard to the prevention of seroma, sutures to eliminate space and tension, the use of fibrin glue, and dissection of the Scarpa fascia have been proposed. However, adoption of these strategies has not been widespread, possibly due to observer bias.
The miniabdominoplasty method is an alternative for some patients who do not require extensive excision of skin and fat and want to avoid a long scar. Although the complication rate is similar to traditional abdominoplasty, there are some specific considerations regarding the aesthetic results of this technique. Dog ear deformities are common with this technique and usually require scar lengthening. Additionally, the most critical aspect of a mini abdominoplasty has to do with the appearance of the belly button.
Surgical time is another factor that has recently received special attention in plastic surgery, given the length of some procedures and the possibility of combining several procedures at the same time. In a retrospective review of 1,753 plastic surgery procedures, operative time was associated with higher complication rates (Level of Evidence: Prognosis, IV). Specifically, procedures lasting 4 hours or more were significantly associated with higher postoperative morbidity, with an odds ratio (OR) of 1.61, accounting for infections, wound dehiscence, skin necrosis, seromas, and hematomas. The risk was even higher for procedures lasting more than 5 hours and more than 7 hours, increasing the RR to 3.05 and 4.71, respectively.
Postoperative consultations provide an opportunity to diagnose complications, even though they may be asymptomatic at certain stages of the recovery process. Maintaining a good patient-doctor relationship is key to treating any complications while maintaining the patient's trust. Complications not only affect medical recovery, but also harm expectations.
There will inevitably be a small group of patients who will not be satisfied with the final cosmetic result. Sometimes this will be caused by surgical difficulties or the occurrence of a complication that compromises the aesthetic result; sometimes the patient's preoperative expectations may simply be too high to meet.
There is an even smaller group of patients who will require repeat abdominoplasty to improve a suboptimal outcome. It is worth noting that such operations have a higher risk of complications and typically result in a slower recovery. Despite this, there is no reason to give up on these tasks, as the results can be significantly improved.
Repeated abdominoplasty (A, B) Preoperative photographs. (C, D) Three months after surgery.
For breast fibroadenoma
If there is a benign neoplasm of this type in the breast tissue, a completely different type of mechanism for the appearance of seroma develops.
If surgery has not been performed to remove the tumor, then the formation of serous fluid is the body's immune reaction to a foreign object inside the mammary gland, which can acquire a malignant etiology and must be urgently removed.
In the case of an operation to excise fibroadenoma, seroma of the postoperative suture is expressed in the form of edema, which subsides in the first 5 days from the moment of surgery (if there are no complications).
Prevention of pathology
The appearance of seroma can be prevented, and this is not difficult to do. The main thing is to strictly follow the recommendations of your doctor.
Immediately after surgery, a bag of salt weighing up to 1 kg should be placed on the surgical suture area.- From the first day, start taking immunomodulatory and antibacterial drugs.
- After surgery, wear compression garments that do not allow the skin-fat area adjacent to the suture to move.
- Minimize physical activity for at least 3 weeks.
As a rule, if these recommendations are followed, the risk of post-traumatic seroma of the surgical suture is no more than 10%.
Moderate appearance of serous exudate should not be considered as seroma. This is normal after surgery. Moisture secretion will stop within the first week. But if the exudate is released intensively, it is necessary to draw the attention of the attending physician to this fact so that he can prescribe treatment.
Originally posted 2018-01-31 08:01:58.
Drug therapy
Treatment with drugs is effective at the initial stage of development of the disease, if there are no signs of extensive swelling and the risk of the inflammatory process spreading to surrounding tissues and organs.
It is recommended to use the following medications:
- Erythromycin is a broad-spectrum antibiotic. Take 1-2 tablets 3 times a day.
- Naproxen is a non-steroidal anti-inflammatory gel based on sodium salts, which is applied to the circumference of the suture 2-3 times a day.
- Meloxicam is an intramuscular injection that has an anti-inflammatory, analgesic and decongestant effect. The optimal dosage is 1-2 injections per day, 5 ml each.
- Kenalog is a corticosteroid for systemic therapy. Has strong anti-inflammatory properties. It is injected into the body intramuscularly 1-3 times throughout the day.
- Ketoprofen is a medicinal ointment based on the active substance carbomer. Apply 2-3 times a day to the postoperative suture and skin surface in the area of edema.
The duration of treatment varies from 5 to 20 days. It is important to remember that the type of antibacterial drug is selected individually depending on the strain of infectious microorganisms detected based on the results of the examination.
The essence of the method is as follows:
At the first stage, I perform laparoscopy and, after isolating the uterine vessels, use soft vascular atraumatic clamps to temporarily block the blood flow in them (RF Patent for invention No. 2407467).
After opening the vesicouterine fold of the peritoneum and lowering the urinary tract, I excise the pathologically altered scar tissue using a monopolar “needle” electrode. To do this, I use a device for dosed electrothermal tissue ligation “LigaSure” (USA). I perform this stage under hysteroscopy control. The surgical field in such conditions is absolutely “dry”; I can clearly see the border between the pathological scar and healthy tissue, as well as all the layers of the uterine wall.
Video from the operating room: Correction of an incompetent scar on the uterus
If it is necessary to remove an endometrioid lesion from the uterine wall, then I use modern ultrasonic scissors, which minimally injures the surrounding healthy tissue of the uterine wall and improves the healing processes in the intervention area.
Next, I perform suturing of the uterine wall with a synthetic absorbable thread “V-lock 180” 0 (Covidien, Switzerland) or “Monocril” 0 in two rows with its peritonization, comparing all muscle layers layer by layer. Good visualization of the surgical field allows this to be done easily and reliably.
The next step is to use modern anti-adhesive barriers, which several times reduce the risk of adhesions in the pelvic area, preserving fertility and the possibility of subsequent births.
At the final stage, I remove the soft clamps from the arteries and completely restore blood flow in the uterus.
The advantages of the new “bloodless” reconstructive metroplasty technique are as follows:
- The operation is performed without blood loss, which allows the pathological scar to be isolated and excised with minimal trauma to surrounding tissue.
- The method allows for reliable suturing of the uterine wound, which is necessary for subsequent pregnancy and childbirth.
The technique is especially indicated for patients:
- Those planning pregnancy;
- With the presence of a niche in the scar zone and the thickness of the myometrium from 1.5 to 2.5 mm;
- With the presence of endometrioid infiltrate in the scar area;
- With concomitant uterine fibroids.
Watch a video of operations performed by Professor K.V. Puchkov. You can visit the website “Video of operations of the best surgeons in the world.”
After laparoscopy, three incisions 5-10 mm long are left on the skin of the abdomen. From the first day, patients begin to get out of bed and eat. Discharge from the hospital occurs on the 2-3rd day.
After surgery, we usually prescribe hormonal therapy for 3-6 months to optimize regenerative processes in the uterus. Dynamic observation by a gynecologist is necessary - examination, ultrasound after 1, 3 and 6 months. Pregnancy after laparoscopic reconstructive metroplasty is possible after 6-8 months. It is advisable to first perform hysterosalpingography - an x-ray assessment of the patency of the fallopian tubes and the condition of the uterine cavity. Depending on the size of the suture on the uterus, childbirth is possible either through the natural birth canal or by caesarean section.
Upon completion of the operation, I make sure to use modern anti-adhesive barriers to reduce the risk of adhesions in the pelvic area.
I have experience of about 3,700 minimally invasive surgical interventions on the uterus, including the correction of incompetent scar on the uterus after cesarean section, the results of which are summarized in the monograph “Laparoscopic operations in gynecology”, as well as in more than 50 scientific publications in various professional peer-reviewed scientific publications in Russia and abroad.
Every year, my team of medical specialists and I conduct up to 40 master classes and seminars on modern aspects of high-tech laparoscopic surgery in Russia, the CIS countries and Western Europe. My seminars on laparoscopic treatment of diseases of the uterus and other diseases are attended by medical specialists from large scientific centers, republican, regional and regional hospitals, and students of postgraduate education faculties.
Alternative medicine
Postoperative suture seroma is a complication that requires drug therapy, but there are still alternative medicine recipes that are still used at home.
The most effective methods of traditional treatment:
1. Aloe compress:
- you need to take 3 leaves of this plant and wash them;
- pass through a meat grinder or food processor, squeeze out the juice, and place the resulting pulp on a gauze cloth;
- apply to the seroma site daily for 2 hours as a compress, each time preparing a fresh portion of homemade medicine;
- the resulting juice is taken 3 times a day, 1 tsp. in 10 minutes before the meal);
2. Bran and honey cake:
- prepared using the specified components in equal proportions, when honey is mixed with bran until a viscous mass is formed;
- applied to the surgical suture, or to skin that has signs of inflammation and swelling;
3. Cabbage leaf:
- has anti-inflammatory and drainage properties;
- It is enough to separate it from the head of the vegetable, rinse it, warm it in a warm room and fix it on the diseased area of the body.
Traditional medicine does not approve of folk remedies, especially when there is an accumulation of serous fluid in the area of the wound surface, which is just beginning to recover after surgery.
Vacuum aspiration
This method of therapy is used in the early stages of accumulation of serous fluid, when there are still no signs of the inflammatory process.
The technology of vacuum aspiration consists of the following actions on the part of physicians:
- the patient receives local anesthesia;
- the surgeon makes a small incision on the skin surface in the area of seroma accumulation;
- a tube of an aspiration device is inserted into the wound cavity, which performs forced pumping of liquid by creating a vacuum;
- As soon as the color of what is being removed changes from golden to ichorous, the procedure stops, the doctor removes the device and applies sterile suture material to the incision.
Vacuum aspiration itself lasts no longer than 20-30 minutes. Due to local anesthesia, the patient does not feel any pain or other unpleasant symptoms. After seroma removal using this method, the healing of the postoperative suture proceeds 2-3 times faster than usual.
Using the drainage system
Treatment of seroma by installing drainage is advisable for use in case of repeated accumulation of serous fluid after its initial removal.
The principle of this type of treatment is as follows:
- the patient receives local anesthesia;
- the surgeon pierces the area of the inflammatory process where the seroma is localized;
- a drainage system is introduced into the wound cavity, which is fixed with a medical plaster;
- the final edge of the drainage is attached to the receiver container, where the accumulated serous fluid is discharged around the clock.
The main disadvantage of the drainage system is the high risk of infection of the wound surface, since the system is replaced once every 2-3 days, during which pathogenic microorganisms can penetrate into the soft tissues and provoke even more extensive inflammation of the postoperative suture.