A mastectomy is surgery to remove all breast tissue as a way to treat or prevent breast cancer. For women with early stage breast cancer, mastectomy may be a treatment option. There is also an option for breast-conserving surgery (lumpectomy), in which only the tumor is removed from the breast.
Choosing between a mastectomy and a lumpectomy can be difficult. Both procedures are equally effective in preventing breast cancer recurrence. But despite all the “aesthetic benefits” of lumpectomy, mastectomy is preferred for some types of breast cancer.
New mastectomy techniques can preserve breast skin and provide more natural-looking breasts after surgery. These techniques are called skin-sparing mastectomies (skin-sparing mastectomies).
Surgery to restore breast shape is called breast reconstruction and can be done at the same time as a mastectomy or during a subsequent surgery at a later date.
A mastectomy is used to remove breast tissue if a woman has been diagnosed with breast cancer or is at very high risk of developing it. A mastectomy can be unilateral, when one breast is removed, or bilateral, when both breasts are removed.
What materials are used for breast reconstruction?
- Implants
- Autologous (own) tissue
- subcutaneous fat and skin (DIEP, SIEA, IGAP, SGAP)
- muscle tissue (LD, TRAM, TUG)
- Their combination
The preference for one or another material depends on the specific clinical situation and the individual characteristics of the patient’s body.
Autologous reconstruction benefits from the point of view of naturalness and aesthetics, since the reconstructed mammary gland, both in shape and consistency, will differ little from the second one.
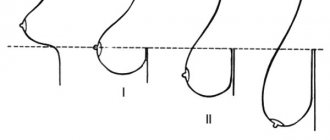
When using endoprostheses, it is necessary to correct the shape of the opposite breast. The breast reconstructed after mastectomy differs from the opposite breast in terms of elasticity, because the implant retains a constant shape.
When the scar resolves
The natural desire after surgery is to look as if the breasts have always been like this without intervention. This will become possible only after at least 2 months . But even then the scar will change, becoming more and more smoothed out and invisible. The whole process can last a year. It also depends on what material was used during the operation:
- If self-absorbable threads were used to fasten the edges of the wounds (which happens with light intervention), they will disappear after 2 - 3 months. There is no need to remove them from the body, but caring for the sutures is still necessary.
- The use of synthetic threads requires their subsequent removal. Of course, the patient is eager to know in advance when the sutures are removed after mammoplasty. This will happen after 7 - 10 days. The doctor will evaluate the condition of the tissue dissection sites, the degree and quality of their healing.
- Haste can lead to the formation of rough, prominent scars, which will then have to be treated. And in the worst case, they may separate, or inflammation may occur in this area.
Removing sutures after laser breast augmentation
Removing sutures can be a little painful . To a greater extent, it depends on the mood of the patient herself. If she is afraid in advance, she involuntarily tenses, which intensifies the negative sensations. But the manipulation itself to remove the suture material is quite fast.
Another sign that causes concern and suspicion that not everything is going as it should is pain at rest and during movement. This feeling is natural, because living tissues and blood vessels were damaged during the operation. It lasts about 7 days. Very susceptible women complain that their stitches hurt after mammoplasty for up to 2 - 3 weeks. If all this time the feeling is decreasing, there are no other alarming signs, it does not indicate anything dangerous.
The pain in the area of the sutures may be stronger due to excessive physical activity of the woman, especially when the upper half of the body is involved (raises the arms, moves the shoulders). Incorrectly selected compression garments can provoke the sensation. In this case, it will need to be changed to a more suitable size.
Watch this video about how stitches are removed and further breast care:
When can you reconstruct your breasts after a mastectomy?
Patient N (p)T1N0M0 on the right, border of the inner quadrants
| Before surgery | 1.5 years after surgery |
After how many days are the stitches removed?
Sutures are removed after mammoplasty and breast lift after 1-1.5 weeks, and for mastectomy, the estimated time frame is 12-14 days after surgery.
After breast augmentation or lift
After breast augmentation or lifting, the sutures are removed for 7-10 days, provided that the postoperative period proceeds without complications (inflammation, seroma, hematoma are absent).
After breast resection
Removal of sutures after breast resection depends on the volume of fluid flowing through the drainage. If it is no more than 50 ml, then the drainage tubes are removed, and after 3-4 days the sutures are removed. Most often this happens 12-14 days after surgery.
Two- and one-stage breast reconstruction
Breast restoration can be two- or one-stage.
Two-stage breast reconstruction using implants is the most popular technique. This procedure can be performed immediately after a mastectomy, or after completion of treatment. The first stage involves the formation of a pocket for a permanent endoprosthesis. To do this, as a rule, a temporary expander (a silicone balloon that is gradually filled with saline solution) is installed under the pectoralis major muscle. Over several weeks, the doctor gradually increases the size of the expander. During this process, the skin and underlying tissue are gradually stretched, creating space for the implant. Over the course of 3-4 months, the volume of the expander is adjusted to the required value. At the second stage, the tissue expander is removed, and a permanent breast prosthesis is placed in the resulting pocket.
One-stage, two-stage reconstruction with expander/implant
| Before surgery T1NOMO, multifocal form | 4 months after expander installation | 2 weeks after replacement with an implant |
One-stage reconstruction – breast reconstruction involves performing reconstruction during one operation. The use of this technique is possible if a woman already has a sufficient musculocutaneous pocket to install a permanent prosthesis and there is no desire to change the size of the gland. One-stage reconstruction is also possible using the Becker prosthesis, which is a combination of an expander and an implant.
One-stage reconstruction, breast implant coverage with LD Flap
- Allows you to fill skin defects
- Completely cover the implant
- Allows you to increase the volume of the mammary gland
| During surgery | Before surgery | 5 weeks after surgery |
Breast reconstruction after removal can also be performed using body tissue - moving and transplanting musculocutaneous flaps (latissimus dorsi flap, TRAM flap) or skin with adipose tissue (DIEP flap and others).
Constant wearing: what to buy
There are four types of products that you will need to create daily comfort in your everyday life.
1. Clothes
Blouses, T-shirts, pajamas, shirts, dresses, tops, sports T-shirts - these products are designed to be worn without a bra because they have a built-in - sewn-in bodice with pockets to support and secure the prosthesis.
2. Bras
The underwear is tailored in such a way that, thanks to the high neckline, a complete fit of the prosthesis is ensured, scars and uneven postoperative surfaces are hidden. Cups with pockets are responsible for reliable fixation and correct anatomical placement of the breast and prosthesis in the bra, without direct contact of the prosthesis with the body. Wide, ergonomic straps guarantee the prevention of lymphedema and relieve stress from the neck and shoulders - with a heavy bust. The high armhole hides tissue deficiency in the armpit area and provides wearing comfort. The wide belt under the chest does not put pressure on the diaphragm, ensuring free breathing and eliminating discomfort in the stomach area.
3. Swimwear
Swimsuits are tailored like bras, have a stylish appearance, and can be either separate or one-piece.
4. Dentures for permanent wear for an attractive appearance
Modern prosthetics provide natural sensations and behavior. They are soft to the touch, sway when walking and “fall off” when lying down. Designed with a special thin edge - it provides a delicate fit in the sensitive seam area and a natural transition to the lines of the body.
These products are made taking into account the various features of the female breast: full-bodied and lightweight, triangular and teardrop-shaped. They also minimally touch the body, so they do not overheat it - there is no increased sweating, and a natural microclimate is maintained.
How is breast reconstruction done immediately after a mastectomy?
First, the surgical team removes the breast. The next step is to form a muscle pocket from the pectoralis major and serratus anterior muscles for an expander (in the case of a two-stage reconstruction) or a permanent implant (in the case of a one-stage reconstruction). The operation is completed by intradermal suturing of the wound using absorbable (biodegradable) materials. There is no need to remove such sutures after surgery.
Delayed reconstruction with an implant with LD Flap cover
How does delayed breast recovery work after removal?
The surgeon excises the old mastectomy scar and sequentially separates the pectoralis major and serratus anterior muscles from the chest wall. This creates a pocket for the expander. An empty expander is placed in the resulting pocket. The muscle pocket is sutured and a drainage tube is installed.
The operation to replace the expander involves the same operational access. The pocket, the capsule formed around the expander, is opened and removed. A permanent endoprosthesis is installed in its place.
With delayed reconstruction, it is possible to reconstruct the breast in one stage. In this case, own tissues or their combination with implants are used.
What else should you do to make the stitches on your chest heal faster?
To make the stitches on your chest heal faster, you need to:
- do not load the shoulder girdle - avoid lifting heavy objects, active movements of the limbs until scar tissue forms (from 15 to 20 days);
- monitor the condition of the wound, treat it with antiseptics, lubricate it with cream as prescribed by the surgeon;
- take a shower in the first month, covering the seam with a bandage;
- be sure to wear underwear with a slimming effect, and you should have at least 2 sets to change to clean ones every day;
- prevent pressure on the seam, do not sleep on your side.
Watch this video about caring for stitches after breast augmentation:
Features of delayed breast reconstruction
This technique can be offered to patients who have completed treatment of the underlying disease or, at least, stages of therapy that require time for the woman’s body to recover.
The disadvantage of delayed breast reconstruction after cancer is that the patient has to live without a breast for a certain period of time. Every woman experiences this differently. To reduce the negative effects of the absence of an organ, it is recommended to use a breast exoprosthesis (an onlay that simulates a breast).
Long-term results of breast reconstruction with DIEP flap
Correction of breast shape after sectoral resection
Restoring the shape of the mammary gland after sectoral resection, as a rule, involves restoration with one’s own tissues. For these purposes, lipofilling is used - a technique for transplanting adipose tissue from other areas of the body that become donor sites. In some cases, it is possible to correct the shape by installing an implant under such a gland. The issue is resolved individually depending on the type of defect, its location and the patient’s physique.
Delayed formation of the nipple-areolar complex
Breast removal: indications, preparation for surgery, complications - MEDSI
Table of contents
- Factors in the development of breast cancer
- Tests and preparation for surgery
- Types of operations
- Postoperative period
- Consequences of mastectomy
- Complications after mastectomy
- Contraindications after surgery
- Advantages of carrying out the procedure at MEDSI
According to statistics, a malignant breast tumor is diagnosed in 1/5 of women who have been diagnosed with cancer.
The number of newly discovered breast cancers per year is at least 55,000. If the disease can be identified at an early stage, doctors use various types of therapy and low-traumatic surgery. If the case is advanced, a mastectomy
— surgery to remove the mammary gland (complete or partial).
Factors in the development of breast cancer
Modern medicine has not yet established the exact causes of breast cancer. But doctors identify several types of factors that can trigger the appearance of a malignant neoplasm:
- The presence of certain types of diseases:
- Diabetes
- Ovarian cysts
- Thyroid dysfunction
- Uterine fibroids
- Hypercholesterolemia
- Endometriosis
- Pituitary gland dysfunction
- Tumors of the female genital organs
- Adenomyosis
- Incorrect functioning of the adrenal glands
- Early menstruation (before 12 years of age)
- Several abortions
- Late labor, absence of labor
- Milk stagnation due to refusal of breastfeeding
- Late menopause (after 55 years)
Tests and preparation for surgery
The doctor prescribes surgery to remove the mammary glands for the following indications:
- Treatment with other types of therapy has not given a positive effect or there are contraindications to them
- The resection process did not completely remove cancer cells
- There are many nodes or cysts
- Extensive purulent inflammation of the mammary gland
- Large tumor size (more than 5 cm or 1 quadrant)
To avoid complications during surgery or identify possible contraindications, the doctor sends the patient for tests:
- Ultrasonography
- Electrocardiogram
- Urine examination
- Complete blood count and coagulation test
- Mammography
- Biopsy
If the oncologist has prescribed surgery to remove the mammary gland, the patient must undergo the following preparation:
- 2 weeks in advance - stop taking blood thinners and other medications (as prescribed by your doctor)
- 12 hours before - abstain from eating
- The night before, cleanse the intestines with an enema, and also receive a set of necessary antibiotics
Types of operations
The operation to remove the mammary glands is performed under anesthesia and can last 1–3 hours, depending on the complexity of the surgical intervention:
- Partial removal of only the affected areas, in some cases along with the lymph nodes
- Subcutaneous removal of the gland along with lymph nodes, but without removal of the nipple and areola
- Complete removal of the breast, including the nipple and areola, excluding the pectoral muscles
- Removal of a quadrant of the cancerous area, with a separate incision to remove lymph nodes
- Radical mastectomy:
- According to Halsted - removal of the mammary gland, both pectoral muscles, axillary lymph nodes, fatty tissue from the armpit, under the collarbone and scapula
- According to Urban - in addition to removing both pectoral muscles, axillary lymph nodes, mammary glands, fatty tissue from the armpit, under the collarbone and scapula, parasternal lymph nodes are also removed
- According to Patey, the gland and lymph nodes are removed in one block, but the pectoralis major muscle is preserved
- Extended - in addition to removing the mammary gland, the pectoralis major and minor muscles, lymph nodes are removed, and a chest resection is also performed
- Advanced - through an incision around the areola, a complete amputation of the gland is carried out, including the small blood vessels of the lymph nodes
Postoperative period
After surgery to remove the mammary gland, rehabilitation lasts about 1.5–2 months. In the first days, severe pain and discomfort are possible. You can start walking no earlier than one and a half days after the operation.
In order for the rehabilitation period to be successful, you must adhere to the following rules:
- Do not make sudden movements
- Don't raise your hands
- Do not try to speed up the recovery of physical activity
- Wear a special bandage on the chest
- It is necessary to regularly go to dressings, during which the doctor can also remove lymph accumulation
- After 2 weeks, the specialist will remove the stitches
- You should do therapeutic exercises prescribed by your doctor.
- It is necessary to protect the hand adjacent to the operated area from injury.
- If there are no complications or other problems with healing, the patient can return to normal life in 1.5–2 months, including the ability to be sexually active
For a more successful rehabilitation period, it is necessary:
- Give a light massage to the arm and shoulder
- After removing the stitches, do light exercises
- Visit a doctor at least once every 3 months, later - once every six months
Consequences of mastectomy
In the first time after surgery, possible negative manifestations such as:
- Tension and roughening of the skin in the surgical area and underarms
- Pain and discomfort in the arms, chest, armpit
- Swelling may develop due to lymph drainage
Such sensations often go away during the rehabilitation period, but in rare cases they can become chronic.
If the patient decides to undergo breast reconstruction surgery, the specialist will prescribe such an intervention no earlier than 9 months or a year after the mastectomy.
This operation will require either the installation of an implant or the transplantation of fatty tissue and skin from other parts of the body (buttocks, abdomen or back).
Complications after mastectomy
After surgery to remove the mammary glands, the following complications may occur:
- The appearance of pus at the incision site
- The occurrence of hematoma or bleeding
- Discomfort and pain in the chest, arms, armpits
- Bacterial infection enters skin and subcutaneous tissue cells
- Stagnation of lymph due to its excessive secretion
- Damage to nerve endings, which is expressed by pain in the shoulder joints, inhibition of movement
- The appearance of pain in the suture area, as well as scars
It is necessary to immediately consult a specialist if the patient exhibits the following symptoms:
- Swelling, tightness and coldness of the hand
- Pain and difficulty moving limbs
- Pallor or blueness of the hands
Contraindications after surgery
During the rehabilitation period, it is strictly forbidden to perform such actions as:
- Before removing stitches:
- Take a bath or shower
- Sleep on your side on the operated side
- Experience physical activity
- Visit the pool
- Experiencing overheating or hypothermia
- Sunbathe
- Do heavy physical activity
Advantages of carrying out the procedure at MEDSI
- MEDSI network clinics use only the latest generation equipment, which allows for accurate diagnosis of mammary gland diseases: ultrasound, mammography, CT, MRI, histology of biopsy results and testing for tumor markers
- MEDSI has the only newest mammograph in Moscow, GE Senographe Essential, which evaluates factors for the development of breast cancer
- Clinic specialists try to use gentle surgical methods, and to treat severe tumors they use an integrated approach: radical resection of the mammary glands with removal of regional lymph nodes in combination with radiation and chemotherapy
- To identify cancer at an early stage, MEDSI uses cancer screening programs based on unique techniques
To schedule a consultation, call: 8 (495) 7-800-500.
Nipple and areola reconstruction
Restoration of the nipple-areolar complex, which plays an important role in giving a natural appearance to the mammary gland, is the final stage of breast reconstruction. It is performed after the complete reconstruction of the shape and size of the breast. The surgeon positions the nipple-areolar complex at the apex of the breast.
This is a technically complex operation and is performed in the projection of the area where the mammary gland with a tumor process was previously located.
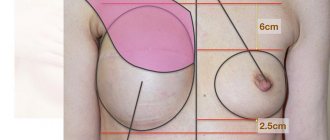
When reconstructing the nipple and areola, their normal positioning and symmetry with the opposite nipple is very important.
Such a reconstructive plastic procedure can be carried out as an independent outpatient intervention, or it can be part of an operation for reconstruction of a removed breast in a hospital.
Since the reconstruction uses skin, the color of which does not differ from the surrounding tissue, medical tattooing is necessary after the reconstruction.
Simultaneous formation of the nipple-areolar complex
Care after mammoplasty
The success of the operation depends on care after mammoplasty: treating the suture with alcohol, Miramistin, other antiseptics, applying healing and absorbable ointments.
How long should scars on the areola be treated with alcohol after mammoplasty?
It is recommended to treat scars on the nipple areola after mammoplasty surgery with alcohol until the crusts covering the wound fall off on their own. Use either alcohol or solutions of iodine, brilliant green at the discretion of the doctor. At the next stage of treatment, absorbable ointments are used.
Wound after breast reconstruction: what cream to use to heal
Your doctor may recommend a cream after breast reconstruction to help the wound heal faster:
- Contractubex – has a softening, anti-inflammatory effect, contains heparin, onion extract and allantoin;
- Dermatix is a silicone gel that smooths out protruding scars and lightens them;
- Imoferase – based on the enzyme hyaluronidase, reduces redness, pigmentation, itching, dryness, moisturizes;
- Vulnuzan – contains salts from Lake Pomorie, has a strong anti-inflammatory and cleansing effect, is used for long-term non-healing wounds;
- Eplan is the active ingredient glycolan, it inhibits the growth of bacteria, relieves pain, stimulates tissue restoration, and relieves swelling;
- Stellanin - exhibits both antimicrobial and wound-healing effects, accelerates the fusion of suture edges during inflammation;
- Mederma - softens scar tissue, prevents keloid formation. A similar result is provided by: Kelocode, Dermofibraze, Dermatix, Contrarubet, Zeraderm.
Creams for healing scars after nipple surgery
After mammoplasty surgery, creams, gels and ointments are recommended for healing scars on the nipples; the most effective ones include: Dermatix, Mederma, Kelofibrase, Contractubex, Imoferase. They are applied after drying and rejection of dense crusts.
How to treat a seam at home with Miramistin
To treat a seam at home, Miramistin is applied to the surface of the skin. It is most convenient to use a spray bottle. First you need to remove the remnants of the bandage covering the wound. If it is difficult to remove, you can moisten it with hydrogen peroxide. Then Miramistin solution is sprayed and left until dry. This drug has a wide spectrum of antimicrobial action and is indicated for the treatment of purulent and uncomplicated postoperative wounds.
Lifting the second, healthy breast (mastopexy)
Mastopexy is the removal of excess skin and giving the mammary glands an anatomically correct position. Symmetrizing surgery on the opposite mammary gland, allowing for correct positioning of it, is an integral part of the comprehensive rehabilitation of patients. It is carried out as an independent intervention, and can also be performed during surgery to remove a mammary gland with a tumor. The operation requires a hospital stay of about three to five days.
A clear result can be seen 2 months after the lift. But even after this, the breast will continue to recover. The final result of mastopexy occurs after 6 months.
Clinical guidelines
- recurrence in the operated breast
If after breast-conserving surgery the tumor reappears in the already operated mammary gland, then the optimal solution would be to remove this mammary gland to prevent the risk of recurrence of the disease.
Under good conditions, the possibility of repeat organ-preserving surgery may be preserved. It is important here that the skin is not affected by tumor cells, and that the primary disease occurred several years ago. To help prevent a recurrence, doctors will check whether you can be considered for more radiotherapy. Radiation is especially recommended if it was not used during primary treatment.
- recurrence in the chest wall area
Recurrence must be re-operated. The goal is complete removal of the tumor. The operation becomes more complicated if the ribs or muscles in the intercostal space are affected. In these situations, treating physicians should seek advice from physicians who specialize in chest surgery. Radiation may then be considered, especially if you have not received radiation therapy before.
- relapse in the armpit
The treating team should repeat oncology surgery in the armpit and, in certain situations, also prescribe radiation therapy after that. If it is not possible to remove it surgically, then irradiation of the axillary lymph nodes can also be performed.
Correction of the reconstructed breast shape
As a rule, lipofilling is used to correct the shape of the breast after reconstruction. Lipofilling (mammoplasty with autologous fat) - procurement, preparation and injection of the patient’s own fat cells into the mammary gland.
These cells partially disintegrate and are excreted, partially remain in the breast, blood vessels grow in them, and fat cells become part of the organ.
Over time, fat accumulates and due to this, the shape of the mammary gland is adjusted or its volume increases.
Increase in original breast size
In patients with breast cancer, after complex treatment using lipofilling, it is possible to improve cosmetic results. After this procedure, you will need to stay in the hospital for one to two days.
Consequences of intervention
Healing of the sutures occurs with the formation of fibroblasts, which eliminate the tissue defect resulting from the incision. An epithelial coating then forms in the wound, preventing bacteria from entering.
Gradually, the edges of the wound are attracted to each other. Thin seams are formed, which, with favorable developments, are hardly noticeable, but are still visible. Carrying out mammoplasty involves their location in such places that prying eyes will be unable to detect its traces.
What is important for good seam aesthetics besides maintenance:
- Age . In young people, healing proceeds faster due to a high ability to regenerate and a more active immune system.
- Normal weight . With its excess or deficiency, recovery occurs more slowly.
- Nutrition . It must be complete to ensure the supply of “building material” for newly formed tissues. Sufficient intake of fluid into the body is also important.
- No bad habits . Alcohol and smoking interfere with the production of new cells.
Result of mammoplasty
Possible complications after breast reconstruction after mastectomy
Breast swelling
Associated with tissue trauma during surgery.
It is recommended to wear compression garments after surgery and avoid thermal procedures and any exposure to heat (in the bathhouse, on the beach, in the bathroom). Physical activity should be avoided for a while. When following the doctor's recommendations, the swelling usually goes away quickly.
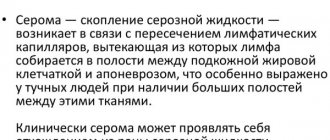
Seroma
Seroma is an accumulation of serous (intercellular) fluid in the surgical area. This complication is associated with the intersection of the lymphatic pathways when removing axillary tissue from the lymph nodes. In the early postoperative period, such fluid flows through drainage tubes. In case of seroma development, after removal of the drains, the fluid is removed from the cavity with a syringe under ultrasound guidance. If the recommendations of the attending physician are not followed, seroma can lead to inflammation.
Hematoma
Sometimes a damaged vessel, in which the blood has clotted, begins to bleed after the operation is completed. In this case, a hematoma forms, an accumulation of blood in the area of the operation - a brown clot above the skin. It manifests itself as a change in the shape and symmetry of the mammary glands, and an increase in breast size.
Pain in the surgical area
It can also be a complication if it bothers you for several months.
Capsular contracture
Deformation of the prosthesis due to the dense fibrous capsule that has formed around it. It is considered the main complication of endoprosthetics.
In case of complications such as tissue contracture in the area of the installed implant, rotation-migration of the implant, severe pain in the projection of the endoprosthesis, repeated surgical intervention is required to correct the shape of the breast reconstructed after surgical treatment of cancer. After this operation, the patient remains in the hospital for no more than five days.
Patients with cancer require an integrated approach to treatment and rehabilitation. Oncologists with experience in such operations help to restore breasts after removal, choosing the optimal method taking into account the individual characteristics of the body. Most interventions on the mammary gland with an oncoplastic component and reconstruction of the shape of the mammary gland occur through subsidies from the Ministry of Health of the Russian Federation (quotas), that is, free of charge for the patient.
Diagnosis for suspected recurrence of breast cancer
If you suspect a relapse, you should immediately consult a doctor. The specialist will conduct diagnostics: examination, palpation, mammography, prescribe ultrasound of the postoperative scar and regional areas and morphological (cytological and histological) examination.
Morphological examination of a recurrent tumor should be carried out similarly to the diagnosis of a primary tumor, including the determination of estrogen receptors (ER), progesterone receptors (RP), HER2/neu, Ki67. Based on the data obtained, further tactics and treatment methods will be determined. If necessary, the oncologist will prescribe additional studies and tests.