What is septoplasty
Septoplasty
- an operation aimed at eliminating
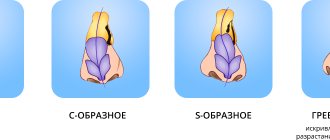
the curvature of the nasal septum
.
Deviation of the nasal septum is observed in 96% of the population, thereby being the most common pathology of the ENT organs. The curvature appears during the growth of the bone and cartilaginous parts of the nasal septum and as a result of injuries to the nose.
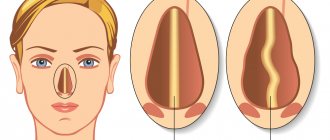
When breathing through the nose, the air in the nasal cavity is moistened, warmed, and disinfected (the mucus produced by the cells of the nasal mucosa has a bactericidal effect). Small villi - cilia of the ciliated epithelium on the nasal mucosa ensure the removal of various biologically active agents: bacteria, viruses, toxins. Thus, humidified, warmed, and disinfected air enters the lower respiratory tract and the cavity of the paranasal sinuses. If there is a curvature of the nasal septum, the above functions may be disrupted due to improper passage of the air stream and its impact on the curvature (spike, ridge).
Indications for surgical treatment
Indications for surgical treatment of a deviated nasal septum are:
- difficulty breathing through the nose
- development of chronic rhinitis
- recurrent purulent sinusitis
- recurrent nosebleeds (if the cause of the bleeding is a deviated nasal septum). When an air stream hits a curvature, irritation and atrophy of the mucous membrane gradually develops in this area.
- development of cysts in the paranasal sinuses due to a deviated nasal septum
- with the development of polypous processes in the sinuses (treatment is necessary to eliminate the mechanical barrier to the passage of medicinal substances into the sinuses for the treatment of polyps)
If you are concerned about difficulty in nasal breathing, recurrent nosebleeds, or there are cases of repeated sinusitis, you should consult an ENT doctor.
In order to determine whether surgical treatment is required in your case, the doctor will conduct all the necessary instrumental studies (endoscopic examination of the nasal cavity, computed tomography of the paranasal sinuses) to exclude pathology in them and prescribe laboratory research methods to exclude the allergic and infectious nature of the difficulty in nasal breathing.
Discussion
One of the key points in the prevention of postoperative complications is the identification of clear indications for surgical intervention, since the diagnosis of PPI is usually not based on objective research data [33]. In this regard, it is advisable to use objective methods for assessing difficult nasal breathing before surgery, for example, anterior active rhinomanometry. It is important to take into account the presence of allergic diseases in the patient and the use of medications, since anticoagulants and herbal preparations can provoke the occurrence of the most common complications such as bleeding and poor healing [16]. If the patient is a smoker, it is advisable to stop smoking for 2 to 4 weeks before and after the intervention due to the fact that smoking may contribute to unsatisfactory healing. It is also important to consider the presence of autoimmune conditions in the patient, as this may adversely affect the outcome of the operation [16].
To reduce the risk of postoperative complications, various techniques are used, the most common of which are nasal tamponade, installation of septal splints and suturing of the nasal septum, however, clinical studies with a large sample are necessary to determine the benefits of a particular method.
In recent years, more and more importance has been attached to the patient’s quality of life in the postoperative period, therefore preference is given to tampon-free postoperative management techniques, which are associated with a lower risk of pain and discomfort for the patient. To date, no consensus has been reached regarding the duration of use of intranasal splints, which ranges from 2-3 days to several weeks. Conducted studies on this issue have not revealed any significant disadvantages of long-term (7 days or more) use of intranasal splints [34], so the surgeon can select the time of use of splints based on the specific clinical situation. Postoperative care for the nasal cavity is also of no small importance: irrigation with saline solutions, the use of healing gels and ointments, and professional toileting of the nasal cavity.
Types of septoplasty
Radio wave septoplasty
Radio wave septoplasty
– the most gentle type of surgical intervention, since the excision occurs in the nasal cavity on the mucous membrane, thanks to this it becomes possible to avoid scars. The advantages of this operation include not only the aesthetic appearance, but also the fact that the postoperative period is not problematic and takes less time. Radio wave septoplasty takes no more than one hour, including preparation for the operation. During septoplasty, the surgeon removes only those parts of the nasal tissue that do not allow the nasal cavity to function normally, so in most cases the integrity of the nasal septum remains unchanged.
Laser septoplasty
Laser septoplasty
performed by equipment that creates a laser beam.
This type of operation produces a great antiseptic effect, so the likelihood of infection or complications during and after the operation is as low as possible. The rehabilitation period passes quite quickly. Laser septoplasty takes no more than half an hour, and hospital stay is no more than a day. But with all the advantages of this procedure, it has a large list of contraindications - you should definitely consult a specialist. Comparative characteristics of radio wave and laser septoplasty
| Radio wave septoplasty | Laser septoplasty | |
| What is used | Surgitron device Videoendoscope | Laser ray Video endoscope |
| Operation duration | Within an hour (depending on the complexity of the curvature). | No more than half an hour |
| pros | The most gentle method Avoiding scars (only curved sections of the septum are removed, the curved cartilage is corrected and returned to its place in a corrected form). Maintaining the integrity of the septum Short rehabilitation period | Great antiseptic effect Short rehabilitation period Short operation time Shortest duration of hospital stay in the postoperative period Shortest duration of hospital stay in the postoperative period (1 day). |
| Minuses | Longer hospital stay | Correction of curvature using a laser is only possible in the cartilaginous part of the nasal septum. Therefore, the method is used much less frequently. Multiple contraindications. |
| Staying in hospital | 3 days | 1 day |
results
An unsatisfactory effect during operations on the nasal septum may be the result of a complication or error. A complication is an undesirable phenomenon, the occurrence of which does not depend on the actions of the surgeon; on the contrary, the error is the result of incorrect planning/execution of the intervention or management of the postoperative period. Often it is not possible to separate these events [4].
Complications during correction of PPI can be divided according to the time of occurrence into intraoperative, occurring in the early and delayed postoperative periods. Depending on the cause, they may be associated with errors in the intervention, anesthesia, as well as decompensation of the patient’s chronic diseases during the intervention or incorrect postoperative care.
The overall incidence of complications during interventions on the nasal septum, according to various estimates, is up to 25% [8]. Long-term complications of traditional septoplasty are observed in 2-10% of cases [4]. The most common complications with traditional septoplasty include: persistent nasal obstruction, bleeding, septal hematoma, perforation of the nasal septum, synechiae of the nasal cavity, infectious complications, aesthetic disorders [3]. Among the complications of endoscopic septoplasty, the following were recorded: transient dental anesthesia/pain, septal hematoma, bleeding, perforation of the nasal septum, abscess of the nasal septum, and the formation of synechiae [8].
When comparing submucosal resection of the nasal septum and traditional septoplasty, a more frequent occurrence of saddle-shaped deformation of the nasal dorsum, drooping of the nasal dorsum, flotation of the nasal septum and perforation of the nasal septum was noted when performing submucosal resection [9]. According to a meta-analysis of 14 studies [8], with traditional septoplasty, bleeding, adhesions, residual deviation of the nasal septum and ruptures of the mucous membrane are more common than with endoscopic; There were no differences in the incidence of nasal septum perforations, infectious complications, nasal septum hematomas and external nasal deformities. When performing interventions on the nasal septum using a laser, the authors generally note the absence of complications, with the exception of residual deviation of the nasal septum.
After analyzing trials in Germany related to septoplasty failures, J. Windfuhr [10] found that they were associated with complications such as anosmia, perforation of the nasal septum, damage to the base of the skull and subatrophic rhinitis.
The type of anesthesia also affects the incidence of certain postoperative complications. Thus, general anesthesia increases the risk of a patient’s re-admission to the clinic after surgery, and the incidence of nausea, vomiting and bleeding is 36, 14 and 3.6%, respectively, with local anesthesia - 8, 3, 0%, respectively [11].
Epistaxis during surgical interventions on the nasal septum is the most common complication, the incidence of which is 6.0–13.4% [11, 12]. Bleeding can occur both intraoperatively and in the delayed period. As a rule, the amount of blood loss does not pose a threat to the patient, however, in the literature there are descriptions of cases of death due to bleeding during surgery on the nasal septum. Thus, A. Koçak et al. [13] describe a case of fatal bleeding from the internal carotid artery after septorhinoplasty.
Factors that increase the risk of developing nosebleeds include: taking anticoagulant and antiplatelet drugs, general anesthesia, coagulopathies and certain types of postoperative nasal tamponade. The addition of low doses of adrenaline to the anesthetic solution when performing hydroseparation, the use of local and systemic hemostatic drugs, as well as controlled hypotension help reduce the amount of intraoperative blood loss. Patients are advised to avoid aspirin, non-steroidal anti-inflammatory drugs, anticoagulants and sports activities for 2-4 weeks after surgery.
A large number of studies have been devoted to studying the effect of postoperative tamponade methods on the likelihood and amount of bleeding after septoplasty. Thus, with standard tamponade, the bleeding rate ranges from 22.9 to 25% [14]. Gauze tamponade, which was previously widely used after endonasal interventions, has now been abandoned by many surgeons, since it is associated with a higher risk of postoperative bleeding than modern methods of nasal tamponade. Removal of a gauze tamponade, especially after installation for 2 days or more, leads to damage to the nasal mucosa, comparable to surgical trauma [15]. Nasal tamponade with elastic tampons, Merocel tampons and similar ones is associated with discomfort and pain for the patient, and therefore methods for tampon-free management of patients after septoplasty are being actively developed. Thus, suturing the nasal septum, using septal splints and fibrin glue did not differ from nasal tamponade with elastic tampons in terms of the number of postoperative bleedings in the studies, but was more comfortable for patients. It is important to note that in these studies, the authors mainly consider the isolated performance of septoplasty without simultaneous operations [16, 17].
The incidence of nasal septum hematoma after septoplasty is, according to various estimates, from 0.7 to 5% [3]. The hematoma itself can lead to complications such as ischemia and necrosis of the cartilage of the nasal septum, as well as a worse prognosis for the success of septoplasty due to displacement of the nasal septum. Along with this, infection of the hematoma with staphylococcus, Haemophilus influenzae or, less commonly, Pseudomonas aeruginosa can lead to the formation of an abscess of the nasal septum [16].
To prevent postoperative hematoma, nasal tamponade, suturing of the nasal septum and septal splints are used. Randomized trials that have recorded the incidence of this complication have found no differences when comparing different postoperative management methods [17]. It should be noted, however, that the sample size of most studies did not exceed 100 patients, which may be insufficient to detect differences given the low incidence of nasal septal hematoma.
A common complication of surgical intervention on the nasal septum is synechiae, which occurs, according to various estimates, in 0.3-7% of cases. Risk factors for the appearance of synechiae include intraoperative ruptures of the mucous membrane, simultaneous interventions on the inferior turbinates and lack of postoperative care for the nasal cavity [4, 16, 17].
In the case of isolated operations on the nasal septum, the incidence of synechiae did not differ significantly when tampons, sutures on the nasal septum or splints were used in the postoperative period [17]. During simultaneous interventions on the nasal septum and inferior turbinates, the use of splints can reduce the likelihood of synechiae due to the mechanical isolation of the nasal septum from the lateral wall of the nasal cavity [18]. Prevention of the formation of synechiae also involves careful postoperative care of the nasal cavity, both on the part of the patient and the doctor.
The incidence of perforation of the nasal septum, according to a study including 3911 patients, ranges from less than 1 to 6.7%, while with submucosal resection perforations occur in 6.91% of cases, and with septoplasty - only in 0.86% [3] .
Most often, perforation is formed due to damage to the mucous membrane on both sides of the nasal septum at the same level. Also, the cause may be septal sutures and the use of splints due to pressure and resulting ischemia and necrosis of the adjacent area of the nasal septum [4]. An increased risk of perforation is observed with excessive use of a coagulator in the area of the nasal septum for intraoperative hemostasis [3].
To prevent persistent perforation of the nasal septum during intraoperative ruptures of the mucous membrane, methods of plastic closure of defects during surgery have been proposed [19]. Randomized trials have found no difference in the incidence of septal perforation after septoplasty using tampons, septal sutures, or splints, but the statistical power of these studies is limited by insufficient sample sizes for such a rare complication [7].
Infectious complications after operations on the nasal septum are not common and range from 0.48 to 2.5%, and the incidence of local infection and abscess of the nasal septum varies from 0.4 to 12% [3]. Complications such as meningitis, brain abscess, cavernous sinus thrombosis, and endocarditis are extremely rare, but transient bacteremia is quite common. Thus, I. Kaygusuz et al. [20] studied venous blood samples from patients undergoing septo- or septorhinoplasty. The authors showed that after surgery, bacteremia was detected in 15%, and in 16.9% after removal of the tamponade.
The question of the need and duration of antibacterial therapy to prevent infectious complications after septoplasty remains controversial. In clinical studies, the incidence of purulent discharge and infectious complications was not associated with the presence or absence of antibacterial therapy in the postoperative period [21]. At the same time, the prescription of antibacterial drugs itself can cause undesirable side effects, as a result of which some authors consider the routine prescription of antibacterial drugs in the postoperative period to be unjustified [22]. The literature describes cases of toxic shock syndrome after septoplasty, which may be associated with the use of outdated methods of postoperative tamponade [23].
The most common aesthetic complications of interventions on the nasal septum include: drooping of the nasal bridge and the development of saddle-shaped nasal deformity [24]. Less common: deviation and widening of the nasal tip, retraction of the columella, collapse of the alar cartilages with the development of nasal valve dysfunction. Complications of an aesthetic nature are often observed, with the risk of developing minor changes ranging from 21 to 39.5%, and severe aesthetic defects ranging from 0.4 to 4.5% [25]. Most of these complications are associated with excessive resection or lysis of the upper parts of the quadrangular cartilage (upper 10-15 mm), as well as displacement or resection of the caudal part of the nasal septum. Pronounced aesthetic changes are usually accompanied by deterioration in nasal breathing. Taking into account the fairly high frequency of aesthetic changes, the authors [25] suggest using photo documentation of the shape of the external nose before surgery for subsequent comparison. Prevention of aesthetic complications of septoplasty involves maintaining the size of the quadrangular cartilage sufficient to support the dorsum and tip of the nose, and using plastic techniques to fix the caudal cartilage of the nasal septum in case of subluxation or severe deviation [24].
Sensory complications include: hyposmia, dysosmia, decreased sensitivity of the hard palate and teeth, and visual disturbances.
Anosmia or hyposmia occurs in approximately 1% of patients after septoplasty [16]. Transient dysosmia may be associated with nasal tamponade after surgery, as well as with the presence of crusts and swelling in the nasal cavity. Along with this, a viral infection in the postoperative period can also lead to impaired sense of smell. Rare causes of dysosmia include damage to small fibers of the olfactory nerve [16]. When planning surgery, a preoperative assessment of olfactory function is important to avoid complaints from the patient.
Impaired sensitivity of the hard palate and teeth is observed in 2.8% of cases with septoplasty [26]. In a study by N. Sautter and T. Smith [27], transient dental anesthesia/pain during endoscopic septoplasty was reported in 7% of cases.
There are descriptions of rare cases of visual impairment. The literature describes a rare case of transient complete unilateral blindness due to retinal artery spasm in a 27-year-old girl after septoplasty [28].
Visual disturbances can occur due to direct damage to the optic nerve in the optic canal, as well as with the use of local anesthetics. In the latter case, when local anesthetics and vasoconstrictors are introduced into the membranous part of the caudal part of the nasal septum or into the nasal turbinates under high pressure, a retrograde flow occurs. At the same time, they can reach the branches of the ophthalmic artery, causing embolism and occlusion of the vessels supplying the ophthalmic artery and, as a result, one-sided blindness. To prevent this complication, it is recommended to inject no more than 10 ml of solution under low pressure, and also not to carry out multiple injections in order to minimize the risk of getting into an arterial vessel [16].
Rare complications of septoplasty are presented in the literature in the form of descriptions of individual clinical cases. The cause of such complications, as a rule, is either a gross violation of surgical technique or unaccounted for anatomical features of the patient.
Rare complications of septoplasty include nasal liquorrhea [29], ear noise, and orbital complications [3, 30]. We describe a case of oronasal fistula in a 55-year-old man with no significant medical history after septoplasty. To reduce the likelihood of liquorrhea and damage to atypically located anatomical structures, it is advisable to perform a computed tomography scan of the nose and paranasal sinuses in the patient in the preoperative period. You should pay attention to the height of the sieve plate. When removing bony sections of the nasal septum in the posterior sections, it is not recommended to make strong pulling or loosening movements with instruments, since this can lead to damage to the cribriform plate. If intraoperative liquorrhea occurs, it is preferable to attempt fistula closure under endoscopic control.
Deviation of the nasal septum after septoplasty can either be a consequence of insufficient intraoperative correction or occur secondary to the postoperative period. Secondary deviation of the nasal septum occurs due to scar changes or injuries in the postoperative period. Secondary deformity varies from 8.2 to 15% of cases [4, 16]. However, it does not always cause clinically significant difficulty in nasal breathing and in most cases does not require repeated surgical intervention. The average time for repeat septoplasty is usually 6.2 years [31]. In 52% of cases, the authors perform septorhinoplasty due to aesthetic changes. Repeated septoplasty is often required when the persistent curvature is localized in the caudal part of the nasal septum [32]. In case of severe post-traumatic deformities of the nasal dorsum, simultaneous rhinoplasty is necessary to install the nasal septum in the median position. When performing septochondrocorrection with a holmium or erbium laser, insufficient correction of cartilage was observed in the range from 4 to 40% of cases [33, 34].
How is the operation performed?
The goal of surgical treatment is to remove the cartilaginous and bone deviated parts of the nasal septum. The curved sections of the cartilage are further remodeled, worn away, as a result of which they become straight and, in this form, are re-implanted back between the layers of the mucous membrane.
During the operation, our blade uses the Surgitron radio wave apparatus to reduce tissue bleeding.
If there is a curvature only in the area of the cartilaginous part of the nasal septum, the operation can be performed using a laser.
The main advantage of the operation in our clinic is the least trauma to tissues, removal of only the curved parts of the nasal septum, and reimplantation of the corrected sections of cartilage back.
Price for nasal septum correction and surgical techniques
The human face is a very complex structure - numerous delicate connections of muscles, ligaments, tissue spaces, bones and cartilage can only be studied by an experienced medical specialist.
This also applies to individual elements of the face - for example, the nose, which has a complex base of bones and several cartilages, covered on top with skin and mucous membrane (inside the nasal passages).
As you know, the nasal passages are separated from each other by a thin septum, but only a fairly small percentage of people have a perfectly even septum (the Latin name for this formation).
Features of the formation of facial tissues, previous injuries and other factors contribute to its curvature, and this, in turn, can lead to far-reaching consequences.
That is why the demand for such an operation as septoplasty is steadily growing in Podolsk, successfully performed by the leading plastic surgeon of the Solei . Feedback from both specialists and patients about the technique confirms the high effectiveness of surgical plastic surgery of the nasal septum.