Almost any burn or injury results in scarring
, which often look unsightly or even impede movement.
Removal of such deformities constitutes a separate area of plastic and reconstructive surgery. As in any field, scar plastic surgery has its own characteristics and secrets. For our readers, we would like to give a detailed account of how and in what cases scar deformities are eliminated. Today we are talking with a plastic surgeon, Doctor of Medical Sciences Natalia Alekseevna Vaganova
, who worked for many years in the Department of Reconstructive and Plastic Surgery of the Institute of Surgery named after. A.V. Vishnevsky.
Natalia Alekseevna, tell us about your experience - how many years have you been involved in the surgery of post-burn scars and how many operations have you performed?
At the Institute of Surgery. A.V. I have been working at Vishnevsky for 28 years. And all these years I have been dealing with post-burn and post-traumatic deformities. She started as a resident at the department of trauma and burns. She also studied graduate school there. Then she was added to the staff.
What problems do patients come to you with?
The main direction of our activity is the elimination of post-burn and post-traumatic deformities and contractures. We do not operate on patients admitted with fresh burns. For this purpose, there is a special department for acute burn injury, where the skin is restored and autodermoplasty is performed. But over time, rough keloid scars, cicatricial deformities and contractures form at the site of burn wounds. This is already an area of our competence.
What other problems, besides post-burn and post-traumatic scars, do you solve?
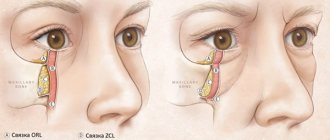
With more complex extensive burns, patients develop various restrictions on the function of movement - contractures. For example, adductor contractures of the shoulder joints, flexion contractures of the knee joints, fusion of the fingers (formation of syndactyly), cicatricial eversion of the eyelids. Such operations are performed first.
In general, if we systematize, we deal with plastic surgery and treatment of all types of scars: burns, post-traumatic, postoperative, we treat keloid scars, we also carry out surgical excision of tattoos...
Let's say the patient had a burn or injury. How long after restoration of the skin after a burn can I come to you for reconstructive surgery?
We usually see patients after 10-12 months, as during this time the scars go through certain phases of maturation.
The first stage is when the scars are bright red, accompanied by itching and pain. In this case, the patient is prescribed physiotherapeutic treatment: ultrasound with hydrocortisone, electrophoresis with Fermenkol, lidase, hydrogen sulfide baths, etc. A year later, when the scar tissue has matured and the scars become flatter and more elastic, we begin surgical treatment.
If we are talking about eversion of the eyelids, then such operations are performed 3-4 months after the acute injury. Since the patient’s eye mucosa suffers due to cicatricial eversion of the eyelid. We also try to eliminate joint contractures at an earlier date due to the development of ankylosis - joint stiffness. Subsequently, we eliminate scar deformities with excision of scars.
Can you say approximately how many operations you have performed during your professional career?
I think several thousand. But I don’t keep an exact count.
Tell us a little about the Institute itself. A.V. Vishnevsky
The Vishnevsky Institute is the country's leading base for the treatment of post-burn and post-traumatic deformities. A lot of research work is being carried out at the institute. We not only operate, but also actively engage in science. On the basis of our department, I defended my candidate and doctoral dissertations. The main direction of my scientific work was the development and implementation of the method of balloon tissue stretching to eliminate post-burn and post-traumatic scar deformities. Our department was the first in the country to use this method.
Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
Burn scars are dense connective tissue formations on the skin that occur when the normal healing of burn wounds is disrupted, as well as when there is extensive and/or deep tissue damage. The main problem for doctors and their patients is hypertrophic and keloid burn scars.
In our company you can purchase the following equipment for the treatment of burn scars:
- UltraPulse (Lumenis)
According to a study of 100 patients with burns (including 59 children), hypertrophic and keloid scars were recorded in 38% of cases, including 34% in adults and 41% in children. Another study analyzed patients in the burns department of Salisbury District Hospital - in 1968, hypertrophic scars were noted in 51% of cases, whereas in 1984 it was already 63% of cases.
The following factors increase the likelihood of developing burn scars:
- young age;
- female;
- localization of damage to the neck and upper extremities;
- more than one surgical intervention in the injured area;
- transplantation of a mesh skin flap into the burn area.
Etiology and pathogenesis
In normal life, most burns occur at temperatures of 100–200 °C with skin exposure lasting more than 1 second. In hot shops and combat zones, burns are possible at temperatures over 1000 °C and exposure time of less than 1 second. The critical level at which thermal tissue damage develops is considered to be 43 °C - temperatures below this value do not cause burns, regardless of the duration of contact with the skin.
The level of local temperature increase in tissues depends on their thermal conductivity - in the dermis it is higher than in subcutaneous fat, since fat is a good insulator. Therefore, thermal damage leading to complete necrosis of the dermis may have little effect on the underlying lipid layer. Although at very high temperatures, not only the dermis and hypodermis are completely destroyed, but also skeletal muscles, fascia, internal organs and bones ( Fig. 1 ).
Hair follicles extend deep into the subcutaneous fat, but this does not always protect them from high temperatures. Although their preservation is critical for rapid and high-quality healing of the injured area.
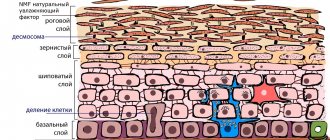
Superficial burns (first level) are thermal damage to one or more layers of the epidermis, with the exception of the basement membrane. The underlying dermis along with the hair follicles also remains intact. Healing of superficial burns usually occurs without scarring, since the bottom of the hair follicles supplies many fresh keratinocytes, which help quickly repair the affected area.
Medium burns (second level) superficial burns of the 2nd level ) or reticular layer of the dermis ( deep burns of the 2nd level are affected . After thermal exposure, macrophages are activated and begin to clean the wound of necrotic debris. Next, fresh granulation tissue forms under the dead tissue, forming the so-called burn scab. All this contributes to the restoration of the epidermis and the formation of a thin normotrophic scar.
With moderate burns, the deep parts of the hair follicles remain viable. The keratinocytes lining their bottom begin to actively divide and migrate to the affected area, promoting reepithelialization. In severe cases, loss of hair follicles may result in insufficient regenerative activity to effectively close the damaged area. If an infection occurs, recovery of the burn wound is delayed and may result in the formation of a hypertrophic or keloid scar.
Deep burns (third level) - thermal damage extends quite deep into the dermis and partially into the subcutaneous fat, where it completely destroys the hair follicle, including its base. Rapid skin regeneration by follicular keratinocytes is impossible in this case - new cells come only from the edges of the wound, so such damage heals slowly. Plus, removing large volumes of necrotic tissue requires long-term work of macrophages. As a result, the likelihood of infection increases, which further complicates and delays regeneration, promoting the formation of hypertrophic or keloid scars.
Main outcomes of burns:
- Healing of a burn wound with complete restoration of the function of the damaged organ or area.
- Healing of a burn wound with partial loss of function of the damaged organ or area.
- Healing of a burn wound with significant loss of function of the damaged organ or area, up to its complete loss.
- The formation of hypertrophic or keloid scars, accompanied by itching, pain, ulceration and severe cosmetic defects.
Rice. 1. Levels of burns and depth of tissue damage
Clinical manifestations
The most severe forms of burn scars are hypertrophic and keloid. Hypertrophic scars are formed as a result of excessive collagen formation - they are dense, rise above the skin level, but do not extend beyond the initial damage and may undergo involution over time. Keloid scars are tumor-like growths of immature connective tissue due to uncontrolled proliferation of fibroblasts. Their peculiarity is rapid growth, accompanied by paresthesia, itching and pain. Keloids can actively increase in size, extending beyond the burn damage to the skin in the form of peripheral strands. They almost never shrink or resolve.
Hypertrophic and keloid scars usually occur in patients with severe (deep and/or extensive) burns ( Fig. 2 ). An aggravating factor is the addition of infection, which significantly slows down the evacuation of necrotic contents and further re-epithelialization. In the area of hypertrophic and keloid scars, pigmentation disorders are often observed - local darkening or blanching, even discoloration.
Burn scars may increase in size over several months and then gradually regress over several years, becoming flat scars without any additional symptoms. However, this scenario does not occur in all patients.
An accurate assessment of the condition of the burn scar is necessary for diagnosis and choice of treatment strategy. Among the various classifications proposed in recent years, the most commonly used is the Vancouver Scar Scale (VSS). In Russia, its modification was developed, presented in table. 1 .
Table 1. Modified Vancouver Burn Scar Scale
| Points | Description |
| By color | |
| 0 | Normally pigmented (color of surrounding healthy skin) |
| 1 | Hyper- or hypopigmented (brighter or paler) |
| 2 | Various shades of red (immature scars) |
| In relation to the level of surrounding healthy skin | |
| 0 | At the level |
| 1 | Below level |
| 2 | Above level |
| By relief and surface quality | |
| 0 | Flat |
| 1 | Lumpy, uneven |
| 2 | With hyperkeratosis and ulcerations |
| By shape | |
| 0 | Scar cord or fold (the length of the scar is greater than its width) |
| 1 | Scar mass (the length and width of the scar correspond to each other) |
Also used in clinical practice are the Manchester Scar Scale (MSS), the Patient and Observer Scar Assessment Scale (POSAS), the Visual Analog Scale (VAS), and the Stony Brook Scar Assessment Scale ( Stony Brook Scar Evaluation Scale, SBSES).
Rice. 2. Keloid scars on the hands after an electrical burn (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/7-55-3.html
Methods
To eliminate the consequences of a burn, conservative therapy or surgical restoration are used. Conservative methods are used as independent treatment only for minor burns, or as an addition to plastic surgery. What are these methods?
- Laser resurfacing The laser resurfacing technique is actively used by cosmetologists and plastic surgeons to treat skin diseases and defects. Using a laser beam, the deformed top layer of skin is “evaporated” and smoothed. In this case, not only the burn site is treated, but also the area around it to ensure a smooth transition. A long course of laser resurfacing, performed by an experienced specialist, allows you to eliminate scars and burns up to 2nd degree.
- Dermabrasion The mechanism of action of dermabrasion is similar to the previous method, but it does not use a laser, but mechanical action with abrasive materials. It differs from laser resurfacing in its low price and lower efficiency. Used to eliminate skin defects, small scars and burns.
- Mesotherapy The mesotherapy method involves the introduction of biologically active substances into the skin. It is rarely used as an independent method of treating burns, so it is complemented by other methods of therapy or surgical operations. When using mesotherapy against burns, doctors choose cosmetic preparations that include antioxidants, vitamins and hyaluronic acid.
With severe burns, not only the skin is affected, but also the muscles, cartilage and other tissues of the face. In this case, conservative treatment methods are powerless - complex plastic surgery is needed, aimed at restoring the shape of the face, facial expressions and skin texture.
To restore facial details - lips, nose and ears, implants are used, which are then fitted with a prosthesis. Technologies for tissue extension, grafting, etc. are also used.
Doctors use skin grafting to restore skin. Transplantation is divided into free and non-free. Free transplantation involves taking skin from distant areas of the body - thighs, back, abdomen, buttocks, etc. A non-free graft involves “tightening” the burn site with nearby skin. If there is not enough skin volume, doctors insert skin expanders next to the burn. Once the healthy skin has stretched, the expander can be removed and plastic surgery performed.
Skin grafting requires a long recovery period. For up to three months, the patient is observed by the attending physician for dressing changes and prevention of complications. Possible complications after skin grafting include:
- Graft rejection
- Infection
- Violation of facial expressions
- Loss of sensation
When transplanting tissue to the scalp, patients often experience a lack of hair growth. To eliminate this problem, hair transplantation from other parts of the body is used.
Restoring the face after a burn can be an expensive, labor-intensive and time-consuming process, but it can achieve results even with third-degree burns, returning the victim to his normal appearance.
Principles of treatment
Treatment of burn scars is a serious problem for a doctor of any specialty. Hypertrophic and keloid scars do not respond well to therapy, so it is recommended to use integrated approaches.
A particular problem is caused by extensive burn scars located in places where the skin should actively stretch - in the bends of the limbs and neck. The presence of such contracture scars leads to limited mobility and a serious deterioration in the quality of life. If the burns were sustained in childhood, this problem is aggravated by the fact that the size of the body increases during growth, but the size of the scar does not. This serious problem requires the use of complex reconstructive surgery techniques.
Generally speaking, the best treatment for burn scars is prevention. It consists of adequate care of the burn wound and preventing the development of infection. This promotes optimal healing without scarring or with the formation of a small normotrophic scar.
When hypertrophic or keloid scars develop, the following treatment methods can be used:
- Pressotherapy using elastic bandages, special knitwear or earrings (for keloids of the earlobe).
- The use of silicone gels under tight occlusive dressings.
- Local application of corticosteroids under occlusion.
- Corticosteroid injections into the scar.
- If the scarring is extensive and/or severe, causing discomfort to the patient or interfering with normal life, surgical excision is possible.
- Using cold to destroy the scar (cryodestruction).
- Laser and other hardware techniques.
A real breakthrough in the treatment of burn scars was the advent of deep fractional ablation . The SCAAR FX scar removal technique is implemented in the Ultrapulse ultrapulse CO2 laser. This device is capable of forming deep (up to 4 mm) but small in diameter (120 μm) ablation microzones in scar tissue. The idea of such an effect is the dosed destruction of scar tissue, which triggers the synthesis of normal collagen. During treatment, only 1-3% of the surface of the scar tissue is destroyed in order to avoid causing the appearance of new scars.
The main goal of the SCAAR FX technique is the gradual, from procedure to procedure, replacement of roughly laid scar collagen with normal collagen with a protein matrix architecture natural to the dermis. The result of this update is a change in the mechanical properties of the scar, giving it flexibility and elasticity, as well as improving its aesthetic appearance.
Questions from our users:
- burn scars treatment
- burn scars laser removal
- post-burn scars treatment
- how to remove post-burn scars
Consultation with a specialist:
Let's talk about these methods then. What is balloon stretching?
The main problem that arises after extensive burns and injuries is the lack of healthy, undamaged skin. To restore the skin, we implant balloons under healthy areas of the skin, which we gradually stretch, and healthy, undamaged skin stretches along with them. The process is reminiscent of the gradual stretching of the skin on the belly of a pregnant woman. The tissue stretching process takes 1-2 months. Plastic surgery is then performed using pre-stretched tissue.
And all this time the patient must remain in the clinic?
The patient can be discharged home or remain in the hospital. During this period, we inject sterile liquid into the expander through the valve tube. Expanders come in various volumes - from 20 to 1200 ml. Depending on the location, the intensity of tissue stretching also varies. For example, when eliminating scarring baldness, the hair-bearing tissues of the head stretch better due to good blood supply. We perform tissue stretching every other day, and sometimes daily. And in implanted expanders on the lower extremities, where the blood supply is much worse, tissue stretching (injection of sterile liquid) is performed 1-2 times a week.
Is this balloon stretching only applicable to post-burn deformities?
This method allows you to eliminate not only post-burn, post-traumatic deformities, but also the method is applicable in reconstructive plastic surgery for oncology. When reconstructing the breast after a mastectomy (partial or complete removal of the breast due to cancer), we implant an expander under the scar tissue, which gradually stretches it. We install a breast implant into the formed pocket. Due to damaged and thinned tissues (radiation, chemotherapy), tissue stretching is performed much less frequently. Therefore, in such cases, we perform stretching once every 2-3 weeks. The entire cycle takes up to several months.
What other scar treatment methods are there besides balloon traction?
There are surgical methods: plastic surgery with local tissues, patchwork plastic surgery, combined plastic surgery and conservative treatment.