Often the first form of nonverbal communication is eye contact. And, as is commonly believed, it is the eyes that can immediately tell a lot about a person: biological age, state of mind and the whole body. Therefore, dark circles under the eyes, sunken eyeballs and deep wrinkles are considered not particularly attractive.
What is the nasolacrimal trough?
At a young age, there is usually no border between the lower eyelid and cheek. However, over time, as a result of shrinkage of the malar bone and downward displacement of the buccal fat pad, the border becomes especially noticeable. A fold is formed running from the inner corner of the eye to the zygomatic arch - the nasolacrimal groove. Correction of this area is usually not required until the age of 35-40, but some require it at a young age. Most often, the early appearance of this defect is associated with heredity, poor nutrition (diet), environmental conditions or ethnicity.
The furrow is further aggravated by dark circles that appear when the skin thins with age, facial muscle weakness, hyperpigmentation, or due to superficial venous tufting.
Precautionary measures
If you think that the nasolacrimal groove can only be removed in a salon, then you should be prepared for any kind of complications. To do this, choose the procedure that interests you and find out as much as possible about it. Read about the procedure, contraindications, reviews, possible side effects and complications. But the most important thing is to treat all information critically. Who knows, maybe a good review was bought?
Non-surgical methods for correcting the nasolacrimal trough
Just a few years ago, it all came down to surgical removal of skin, muscle, fat and blepharoplasty. Today, all techniques for eliminating aesthetic problems have evolved, and more recently, cosmetologists have appreciated the need to restore orbital volume as part of an overall rejuvenation strategy. Non-surgical methods are aimed at improving the overall condition of the skin, and not at masking a specific flaw.
Today, among the non-surgical methods for correcting age-related changes in the infraorbital area, the most commonly used are:
- Mesotherapy (in the early stages and in complex therapy)
- Treatment with fillers
- Hardware correction methods (laser therapy)
Correction of the nasolacrimal trough using mesotherapy
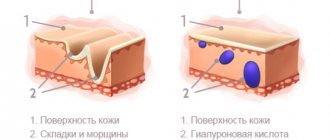
Mesotherapy is carried out using drugs whose main active ingredient is hyaluronic acid. This compound is formed in the human body. Its ability to retain large amounts of moisture is the main property used in aesthetic medicine. After mesotherapy sessions, due to additional hydration, the skin is tightened, regeneration processes are launched, and its protective properties are increased, which last up to 8-12 months. Separately, these drugs are effective in the initial stages of furrow formation, and in combination with fillers and hardware injection techniques, they enhance and prolong their effect.
Prevention
Preventing the development of a nasolacrimal trough is quite simple, but it requires daily effort. Experts recommend:
- limit the consumption of fatty, sweet, salty foods, saturate the diet with fruits and vegetables;
- treat chronic pathologies in a timely manner;
- regularly do facial massage and gymnastics;
- take good and regular care of your skin, use decorative cosmetics in moderation, pay attention to the quality of the products;
- Drink plenty of clean water throughout the day and avoid dehydration;
- add at least minimal physical activity to your daily schedule - walking, light exercise, etc.
Even if there is already a nasolacrimal groove on your face, do not despair. This is just a cosmetic flaw that can be successfully removed with the help of a professional cosmetologist or plastic surgeon.
Correction of the nasolacrimal trough with fillers
Although aesthetic medicine specialists call this area the most difficult to correct, it is the introduction of fillers, like a surgeon’s scalpel, that helps to correct the defect efficiently and permanently. For these purposes, fillers based on hyaluronic acid are used. They fill missing volumes, restore tissue, maintain water balance in the dermis and its normal condition, and also easily dissolve and are removed naturally without any consequences.
Currently, all hyaluronic acid fillers are produced by bacterial fermentation and stabilized by chemical cross-linking. Fillers differ in concentration (density) and particle size. Depending on the condition of the tissue, the doctor, during a personal consultation, determines the type of filler to be used and the method of administration: using needles or a cannula (a long flexible needle with a hole at the end).
How long does the result last after injection with fillers? The effect of fillers in this area can be assessed immediately by comparing photos before and after correction. The result lasts up to 15 months. This long period is a consequence of the relative lack of soft tissue movement in the infraorbital region (compared to the nasolabial folds or lips).
It is worth especially noting that the injection of filler is one of the safest and most effective procedures in aesthetic medicine, but work in the paraorbital area requires special experience and caution from the cosmetologist who performs the injections. The use of non-original drugs and insufficient qualifications of the doctor performing the procedure are the reasons leading to all sorts of complications. This may be swelling that does not go away for a long time, a change in skin color, the appearance of bumps in the nasolacrimal groove and more severe consequences, including tissue necrosis. Therefore, it is very important to choose the right clinic that uses only certified drugs and a highly qualified specialist with sufficient experience.
The term “tear trough” was coined in 1969 by Flowers to refer to infraorbital depression that occurs due to hypoplasia of the zygomatic bones. We use the term "tear trough" to refer to the dark-colored recessed area along the medial aspect of the orbital rim. In this article we talk about the anatomical features of the structure of the tear trough from the perspective of injection correction.
Why does a tear trough appear?
The skin in the lower eyelid area is thin and transparent.
The purple tint of the orbicularis oculi muscle (m. orbicularis oculi), which is located directly under the skin, shines through it. The dark shade of the orbicularis oculi muscle in the area of the lower eyelid is all the more noticeable because there is no subcutaneous fatty tissue in the area of the tear trough. Thus, the main reason for the appearance of the tear trough, in our opinion, is the lack of subcutaneous fat. It is this phenomenon that explains the displacement of soft tissues and the dark shade of the area.
We observe a distinct “interruption” of the superficial malar fat along the outer edge of the tear trough. This distinction is permanent and does not depend on age: the skin in the lower eyelid area contrasts with thicker and lighter skin in the cheekbone area. Val Lambros named this demarcation of the palpebral-zygomatic skin from the palpebral skin lid-cheek junction1.
The direct attachment of the orbicularis oculi muscle to the bone at the level of the arcus marginalis - while the rest of the muscle is free - promotes tissue displacement, and the color of the muscle aggravates the aspect of dark circles [Fig. 1].
Internal palpebral sac [Fig. 2] also participates in the formation of the tear trough:
- raised border: the internal palpebral sac emphasizes the retraction in the area of the tear trough;
- color contrast: bright yellow of the internal palpebral sac and purple attachment of the orbital portion of the orbicularis oculi muscle to the bone.
Finally, infraorbital fat, the so-called SOOF (Sub Orbicularis Oculi Fat), is involved in the formation of the tear trough. The superior edge of the SOOF runs along the edge of the orbit. The lower anterior edge is limited by the attachment point of the muscle that lifts the upper lip (m. levator labii superioris). The lower posterior edge of the SOOF covers the bone attachment and proximal portion of the zygomaticus major and zygomaticus minor muscles. SOOF adds volume: this phenomenon creates a contrast with the recessed area and emphasizes the hollow effect that characterizes the tear trough area. The SOOF ends where the tear trough begins [Fig. 3].
Rice. 1, 2, 3
Thus, the tear trough is an area of depression of dark-colored skin located at the level of the inner part of the edge of the orbit.
The recessed area is a consequence of the direct attachment of the orbicularis oculi muscle to the bony margin of the orbit and the absence of underlying fat and subcutaneous tissue. The tear trough is bounded by two raised projections. Internal palpebral sac on top and superficial malar fat, covered with thick skin, below. The dark color of the tear trough is explained by the fact that the skin of the lower eyelid is thin and more or less pigmented. The second reason is the absence of subcutaneous tissue, which enhances the dark shade of the orbicularis oculi muscle, which is adjacent to two light zones.
Why does the tear trough increase with age?
As a result of age-related changes, the tear trough becomes more noticeable and deeper. This occurs due to changes in the skin itself (atrophy and pigmentation), the appearance or enlargement of the internal palpebral sac and retraction of the inferior orbital edge and subsequent retraction of the muscle attachment, which leads to increased depression. These age-related changes highlight the effect of hollowness and dark circles under the eyes.
Rice. 3
With age, the tear trough becomes more noticeable and deeper due to atrophy and pigmentation of the skin, the appearance of an internal palpebral sac and retraction of the inferior orbital edge and subsequent retraction of the muscle insertion.
Risks of damage to anatomical structures
When correcting the tear trough, there is a risk of damage to the following anatomical structures:
- angular artery (a. angularis);
- infraorbital nerve (n. infra-orbitalis);
- facial nerve (n. facialis).
First of all, the angular artery (a. angularis), the terminal branch of the facial artery (a. facialis) [Fig. 4]. It crosses the midbuccal groove towards the internal canthus, making its way above and below the orbicularis oculi muscle. Thus, there is a risk of damage to the angular artery at the level of the midbuccal groove (at depth) and at the level of the inner part of the tear trough (at the surface). The angular artery reaches the interglabellar region (glabella), crossing the muscle that lowers the eyebrow (depressor supercilii) at the site of attachment of this muscle to the bone (in two places). The angular vein (v. angularis) follows the angular artery.
The infraorbital nerve (n. infra-orbitalis) is located five mm from the bony edge of the orbit under the muscle levator labii superioris (m. levator labii superioris), and slightly mesial to the midpupillary line. In other words, the infraorbital nerve is located above the area where the tear trough is corrected.
The facial nerve (n. facialis) does not pose a real danger, since it has a plexiform structure until it intersects with the circular muscle of the eye (m. Orbicularis oculi), with the muscle that lifts the upper lip (m. Levator labii superioris), and with the muscle that lifts the wing nose (m.levator alaeque nasi). Thus, the facial nerve passes well below the area of tear trough correction.
Important - the tear trough area has a low risk of damage to anatomical structures.
Injection technique
The patient is in a sitting position [Fig. 5]. Before the procedure, the correction area is marked, noting the zone of maximum depression along the entire length of the area. The primary puncture point corresponds to the extreme lateral point of the marked area and is marked with a cross.
Correction is carried out after antiseptic treatment of the correction area with strict adherence to aseptic rules. We use benzalkonium chloride to disinfect the correction area. For local anesthesia of tissues from the epidermis down to the periosteum, inject a 1% solution of lidocaine with epinephrine. Remember that pain associated with injection correction is a deterrent for patients.
The size of the needle for the initial puncture should exceed the size of the cannula by 1G. Note that the needle not only perforates the skin for insertion of the cannula, but also creates depth and direction for the cannula [Fig. 6].
To correct the tear trough area, we use a 25G cannula, the diameter and relative rigidity of which allow us to:
- control the direction: the tip of the cannula always remains along the axis of the syringe;
- control the location of the cannula: the tip of the cannula is palpable, despite the depth of passage of the cannula.
Rice.
5, 6 The cannula is advanced from the palpebral-malar junction to the inner corner of the eye, along the periosteum, from the deep surface of the infraorbital fat (SOOF) to the attachment of the orbicularis oculi muscle to the bone [Fig. 7 – 8]. The cannula slides along the periosteum, without the risk of retroseptal injection, since the concavity of the bone and the partial rigidity of the cannula prevent the cannula from advancing towards the orbital septum.
Hyaluronic acid is released through the lateral opening on the reverse stroke of the cannula after reaching the medial portion of the tear trough [Fig. 9]. Thus, hyaluronic acid is injected into the area where the fibers of the circular muscle of the eye (m. Orbicularis oculi) attach to the bone.
Rice. 7, 8
During the first procedure, you should not inject more than 0.5 ml of filler on each side. We recommend using medium to low cohesive fillers.
The tear trough area has a low risk of damage to anatomical structures. When performing correction, attention should be paid to the angular artery, infraorbital and facial nerves.
The correction does not require massage at the end of the procedure, since the maximum amount of gel is introduced at the level of the bone edge. Therefore, excessively intense massage may result in filler migration from the primary injection site, minimizing the correction effect, or increasing the retraction effect due to the migration of hyaluronic acid above and below the tear trough area.
Rice. 9
After the procedure, the correction area is cooled with a cold pack for 5 minutes to reduce swelling and bruises.
Pain sensations are minimal. If pain occurs while advancing the cannula, it is due to the initial puncture not being deep enough. In this case, a new puncture with a needle should be performed. An identical procedure is performed on the other side. After correction of the first side, the cannula should be placed on a sterile area on the manipulation table.
The results of the correction are monitored 3 weeks after the first procedure. An additional injection may be required: a deep injection of an identical drug or a superficial injection of low-cohesive filler to correct residual surface defects in the area between the lower palpebral sac and the correction area.
Indications for correction
Patients with a negative vector between the ciliary margin and the depressed area. Patients with reduced elasticity of the skin of the lower eyelid, which is checked by a skin elasticity test. The duration of the correction is sometimes several years.
Conclusion
Injection correction of the tear trough allows you to achieve a noticeable aesthetic result: complete filling of the depressed area and partial color correction of the tear trough area.
Authors: Patrick Trevidick, MD, specialist in the field of plastic, reconstructive and aesthetic surgery, scientific director of the international scientific community of surgeons and cosmetologists “Expert2Expert” and the international congress on anti-aging and facial plastic surgery FACE 2 [email protected] , Paris. Thierry Lemaire, MD, specialist in plastic, reconstructive and aesthetic surgery, member of the international scientific community of surgeons and cosmetologists “Expert2Expert”, Paris.
Magazine: Appearance. Esthetic guide №2(25)
Laser correction of the nasolacrimal groove
Laser correction of aesthetic inaccuracies using the Fotona device as part of a 4D rejuvenation program or treatment of only the infraorbital zone is especially popular. As a result, thanks to the use of several unique modes, the elasticity and firmness of the skin increases, it thickens and contracts, the number and depth of wrinkles decreases, and the orbital ligament is lifted.
It is worth noting that today only the Fotona device offers the possibility of tightening the oral mucosa and the lower eyelid mucosa. Thus, deeper connective tissue structures are worked out, collagen production is stimulated and skin elasticity increases.
How long does the effect of laser treatment last? After sessions on the Fotona device, tissue renewal and regeneration processes are launched, which “work” for 6 months. The effect lasts up to 12 months.
Ultrasonic lifting?
Ultrasonic lifting has a prolonged effect, the effect lasts for several years. It is based on the effect of forming a subcutaneous frame at a depth of up to 5 mm due to thermal burns that cause ultrasonic waves. When a patient develops “fat gaps” due to low skin tone, doctors recommend surgical correction.
How painful are the listed techniques?
Most often, these procedures occur without complications, and no recovery time is required.
It should be noted that filling with fillers and mesotherapy are injection methods, so there is always a risk of hematoma formation, which goes away without additional treatment and does not affect the final result.
In mesotherapy, local anesthesia is used only for patients with increased pain sensitivity. In general, injection procedures are moderately painful and most often do not cause discomfort to patients.
Laser treatment is a painless thermal procedure, but the area during treatment is additionally cooled with a special Zimmer device to prevent tissue overheating.
Advantages
Contour plasty has several significant advantages over surgical blepharoplasty.
- No preparation required. Correction can be carried out immediately after examination and consultation.
- The procedure takes a minimum of time. After 30–60 minutes you can leave the clinic.
- Low morbidity. Injection procedures are minimally invasive and involve minimal disruption of the integrity of the skin. Accordingly, the risk of complications tends to zero.
- No traces. Tiny punctures heal quickly, leaving no marks, marks or scars.
- Fast recovery. Redness and swelling persist for a maximum of 3 to 4 days.
- Availability. The number of contraindications is minimal, and the cost is much lower than with surgery.
Contraindications to laser correction of the nasolacrimal trough are:
- Skin and cancer diseases
- Acute and infectious diseases
- Inflammatory eye diseases
Dermatocosmetologists at the Neo Vita clinic have extensive experience in performing such manipulations. All our specialists are certified to work with the relevant drugs and constantly improve their qualification level. Moreover, they themselves are active trainers, training other doctors as part of professional cosmetology events. In their practice, they use exclusively original drugs that have passed state registration.
Thanks to an integrated approach, the clinic not only solves aesthetic problems, but also helps maintain youthful skin for many years.
Side effects and contraindications
If the injection technique is performed carelessly and the advice of a cosmetologist is neglected, infection, movement of the gel, swelling, pain in the area of drug administration, and an allergic reaction may occur.
To prevent unwanted consequences, the procedure should be performed only by qualified specialists and take into account possible contraindications, which include:
- infectious processes in the acute phase,
- pregnancy and lactation period,
- oncological diseases,
- inflammatory phenomena in the injection area,
- epilepsy, etc.