Restoring nasal breathing after rhinoplasty is a question that worries the vast majority of patients. Previously, at the final stage of the operation, plastic surgeons inserted sterile bandages tightly twisted into many layers into the patients’ nostrils. This design was called turunda. Taking out the turundas was very painful, and breathing through the nose with them, for obvious reasons, was impossible. Before removing the turunda, breathing was carried out only through the mouth - both day and night. And there was no way to ease or neutralize the discomfort.
Today, the tactics for maintaining the shape of the nose have radically changed, and therefore, the specifics of primary rehabilitation have changed.
After rhinoplasty
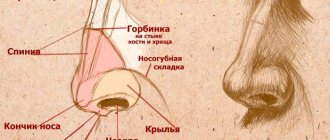
Rhinoplasty is a plastic surgery that corrects imperfections in the nose. This is one of the most popular procedures. This is largely due to the fact that nose surgery is done not only for aesthetic desires, but also for medical reasons. There are a number of features in the structure of the nose (congenital or acquired) that can seriously affect a person’s overall health. And therefore requires the intervention of specialists.
As my practice shows, any patient immediately after surgery begins to inquisitively examine his face. Are there any changes already? Is the nose the way I wanted?
And even though you can’t see anything because of the plaster cast, that doesn’t stop anyone. Premature conclusions are being drawn. And the worries begin.
Let me remind you that immediately after the procedure, the only thing that is reflected on your face is the body’s reaction to the intervention. Swelling and bruising make it difficult to assess changes.
And even after removing the bandage and disappearance of external manifestations, it is too early to judge the results.
Only six months after rhinoplasty will the nose take its final shape.
What happens to the tip of the nose?
In the first months, slight swelling may persist. Therefore, the tip of the nose will appear slightly upturned. In some cases, patients worry that the nose has become too upturned.
But over time, the swelling will subside completely. The swelling will go away. Your nose will become more graceful. It will look thinner. Will decrease slightly in length. And the tip of the nose will drop a little.
In each specific case, only a specialist can understand whether the nasal tip is actually drooping. Because only the doctor knows what manipulations were performed on your nose. And what are the associated features of the rehabilitation period.
If rhinoplasty is done well. If there were no complications during the rehabilitation period. The tip of the nose will drop about three millimeters.
Bruises after rhinoplasty
Breathing after plaster removal
Immediately after the operation, a plaster bandage is applied to the nose, the main purpose of which is to protect the nasal skeleton from trauma. The cast will be removed approximately 7-10 days after rhinoplasty. However, this interval depends on the individual characteristics of the patient and the complexity of the operation.
Many operated patients' breathing improves after this manipulation. This is achieved by reducing pressure on the nose. However, if your breathing has not returned to normal, you should not be upset, you need to be patient, because you are in the process of rehabilitation, or rather, its early period. At this time, the swelling is still clearly expressed, and it significantly complicates the breathing process.
About three weeks after rhinoplasty, most patients regain normal respiratory function. Some begin to breathe fully after the removal of the cast, some after the removal of rhinological splints. Improvement in nasal function is mainly due to decreased swelling after surgery.
The doctor may advise you to use cold compresses during this period, or the use of anti-inflammatory or anti-essudative drugs. Vasoconstrictor drops can alleviate the condition, however, remember that their abuse can lead to addiction. Wound healing medications will also help ease the recovery process.
Why does the tip of the nose droop?
First of all, I note that drooping of the tip of the nose is not a doctor’s mistake or a defect in the procedure. This is a natural stage of postoperative recovery of the body, associated with the behavior of tissues after the intervention.
There may be several reasons for drooping of the tip of the nose after rhinoplasty:
- Natural recovery process
The tissues have taken root in the new place, the consequences of the operation (swelling, bruising) disappear, and final changes in the nose occur. If the procedure made major changes, the likelihood of omission is higher.
- Age
If the patient is under 18 years of age, the specialist cannot guarantee a good result.
If the patient is over 45 years old, the consequences of the procedure can be unpredictable. Dropping of the tip occurs more often in this case. Due to age-related changes in body tissues.
- Changes to be made
For example, removing a hump visually lowers the tip of the nose.
- Type of transaction
With the open method of plastic surgery, the columella is dissected. Therefore, omission occurs much more often. Moreover, it can reach 5-7 mm and be accompanied by the appearance of drop-shaped growths.
- Features of leather and fabrics
If the patient's skin is thick, rough, or problematic, the tip of the nose may drop lower than expected.
If the patient has an overgrowth of connective tissue, this will also affect the degree of drooping of the nasal tip.
How to reduce swelling and bruising
At first, when the swelling is most pronounced, you just need to be patient. The doctor will recommend medications and additional procedures that help reduce swelling for a few hours. But while the tissues are healing, they will not go away completely.
To relieve swelling after rhinoplasty, there are a number of recommendations that should be followed from the first days and at each stage.
Key recommendations in the first week of rehabilitation:
- swelling goes away faster with rest and sleep in a semi-sitting position;
- in the first week you should not massage or put pressure on your face or use cosmetics;
- it is important to exclude elevated temperatures (beach, saunas, hot baths);
- sharply limit any physical activity, especially with sharp tilts of the head or body forward and down.
In the second or third week of recovery, it is important to:
- Avoid sleeping on your side or stomach, especially with your face in the pillow;
- avoid sudden displacement of the skin and underlying tissues on the face (massage, overload);
- avoid exposing swollen areas to heat;
- limit physical activity to household chores only.
The doctor may recommend ointments, gels with decongestant, anti-inflammatory components.
During the second or third month after surgery, swelling remains in the area of the back or tip; for a speedy recovery, doctors recommend giving up smoking and drinking alcohol, and putting pressure on the damaged tissue with glasses, fingers, and various objects. You should also avoid prolonged tilting of your head forward and down.
If by the 4th month the tissues are still swollen, a course of physiotherapy prescribed by your doctor will help relieve nasal swelling after rhinoplasty.
Surgery on the tip of the nose
All of the above applies to nose surgery that does not affect its tip. That is, for those cases when the lowering or raising of the tip of the nose was not planned as a result of the correction.
There are operations to correct the tip of the nose directly. This is one of the most difficult types of rhinoplasty. Such changes can be trusted only to professionals who thoroughly know the specifics of a surgeon’s work in this area. Only in this case the result will be the same as you would like.
You can sign up for a consultation by following the link.
The functional consequences of rhinoplasty can be determined by unpredictable factors, such as the specific features of the repair process, the condition of the skin and its elasticity, the complexity of the deformity, etc. However, most often they are directly and directly related to the surgical technique.
During the evolution of the facial skeleton from animals to modern humans, the nose remains the most protruding part of the skull, which is associated with the function of smell and the need to lengthen the path of inhaled air in order to warm and moisten it [1, 2]. According to I.B. Soldatova [2], distinguish between the main (respiratory, protective and olfactory) and secondary (facial, lacrimal, gustatory, excretory and speech) functions of the nose. G.Z. Piskunov and S.Z. Piskunov [3] added reflex and suction to the listed functions.
A.E. Belousov [4] distinguishes 2 main functions of the nose: respiratory and aesthetic, as well as the phylogenetically fading secondary sexual function. In turn, he divides the respiratory function into olfactory, moisturizing, filtration, resonator (speech) and temperature control functions, which is somewhat unusual from the point of view of traditional otorhinolaryngology. The author considers compliance with the ideals of society, the patient’s ideas, criteria of symmetry and standards of harmony to be an aesthetic function. All of these functions can be disrupted during rhinoplasty.
A.S. Lopatin [1] in his monograph highlights respiratory function, air conditioning, protective (which includes mucociliary transport) and reflex activity, olfactory function with the vomeronasal organ. Let's take a closer look at the possible impact of rhinoplasty on each of these functions.
Respiratory dysfunction.
Reduction rhinoplasty is known to reduce the cross-sectional area of the nasal passages. J. Sheen [5], examining patients for secondary rhinoplasty in the 60-70s of the last century, was convinced that with the operating techniques characteristic of those years, narrowing of the nasal vestibule was present in 80% of cases. M. Constantian [6] described failure of the external nasal valve due to displacement of the lateral limb of the inferior lateral cartilage. This has been noted in cases of primary and secondary rhinoplasty, as well as in cases of skin deficiency in the nasal vestibule.
It is known that postoperative respiratory failure in 70% of cases is a consequence of reduction rhinoplasty. It is also believed that nasal obstruction may be caused by scarring and decreased sensitivity of the mucous membrane. Breathing disorders can be caused by the formation of adhesions and synechiae between the nasal turbinates and the nasal septum. E. Courtiss et al. [7] examined the physiology of the nose in patients undergoing rhinoplasty and found that as long as the external or internal nasal valves are not damaged during the operation or perforation does not occur during a simultaneous operation on the nasal septum, aesthetic rhinosurgery does not affect the nasal breath. Taking care of the physiology of the nose, the authors brought the bones of its pyramid closer together cranial to the internal valve, which supposedly did not worsen nasal breathing. B. Guyuron [8], on the contrary, believes that deep osteotomies can clinically significantly narrow the piriform aperture.
According to G. Beekhuis [9], 10% of patients after primary rhinoplasty complain of residual and new problems with nasal breathing. Other authors believe that in 70% of cases of revision rhinoplasty, nasal obstruction is caused by residual deformation of the nasal septum and stenosis in the area of the nasal valve [10]. Valve dysfunction is usually associated with separation of the superior lateral cartilage from the nasal septum and can be diagnosed using acoustic rhinomanometry [6].
M. Constantinides et al. [11] studied the long-term results of open cosmetic rhinoseptoplasty and its effect on nasal breathing in 27 patients. Plethysmography data (a method for assessing airway patency) in 23 patients showed improvement in breathing and in 4 - deterioration. Moreover, the subjective impression of patients did not correlate with objective measurements. The authors conclude that "...patients with normal preoperative nasal impedance values may have asymptomatic increases in nasal impedance values after cosmetic open septorhinoplasty."
The list of anatomical defects that narrow the nasal cavity and complicate nasal breathing after rhinoplasty can be presented as follows: excessive narrowing of the bony vault; incomplete elimination of deviations of the nasal septum, especially curvature of the caudal region; divergence or spreading of the bases of the medial legs; columella too wide; unresolved hypertrophy of the inferior turbinates; excessive narrowing of the upper lateral cartilages; deformation of the middle vault of the nose; weakness or collapse of the wings of the nose, excessive excision and narrowing of their bases; loss of support and age-related ptosis of the nasal tip; concavity of the lateral crura [8].
In general, according to existing publications, the causes of postrhinoplasty breathing disorders can be divided into several groups. Let's take a closer look at them.
Dysfunction of the external nasal valve.
The external nasal valve is formed by the lateral crus of the alar cartilage, its medial crus, the caudal edge of the nasal septum, the most anterior part of the maxillary ridge, and the soft tissue connecting the lateral crus of the alar cartilage with the edge of the pyriform foramen [12]. Other authors [13] include the alar cartilage, fibro-fatty tissue of the nasal wing, the caudal edge of the nasal septum and the bottom of the pyriform opening as the elements that form the external nasal valve. According to A.E. Belousov [4], the cross-section of the external nasal valve is the lumen of the nostril, which is relatively wide and has more rigid walls compared to the internal nasal valve. E. Huizing and J. Groot [14] consider the external nasal valve as the entrance to the vestibule of the nose, limited by the caudal edge of its septum, the lower lateral (ala) cartilages and the tissue connecting them to the pyriform opening.
The causes of dysfunction of the external nasal valve during rhinoplasty can be a large volume of resection of the alar cartilages, incomplete restoration of the integrity and strength of the lateral crura, lack of careful comparison and suturing of the skin wound, insufficient postoperative compression of the wings with a plaster or plaster bandage to prevent swelling and hematoma, scar changes in the area nasal vestibule and deformation of the columella as a result of displacement of grafts [14, 15]. It is obvious that the recently increasingly used resection of the base of the nasal wings to correct the nostrils (base resection) also leads to a narrowing of the area of the external nasal valve [15, 16].
Dysfunction of the internal nasal valve.
The internal or “true” nasal valve refers to the opening formed by the caudal margin of the triangular cartilage and the cartilage of the nasal septum. It is believed that the internal nasal valve should have an angle of about 15°. Periodically, the lower border of the valve is the anterior end of the inferior turbinate, which increases due to blood filling due to the nasal cycle. The rounding of the caudal edge of the triangular cartilage (scroll) plays an important role in the expansion of the nasal cavity at the level of the valve and helps to increase the flow of inspired air [16].
The internal nasal valve is located at the junction of the relatively narrow nasal pyramid and the wider caudal part of the nose, so any reduction rhinoplasty has a negative effect on valve function. Thus, lowering the nasal dorsum and narrowing the base of the nasal pyramid destabilize the triangular cartilages (including through the mechanism of relaxation of the skin covering them), which impairs the support of the outer wall of the internal nasal valve [14]. With reduction plastic surgery of the caudal part of the nose, the same thing happens with the second cartilaginous element of the outer wall of the valve - the inferolateral cartilage. After all, almost no operation to correct a bulbous nose is complete without removing the cephalic edges of the lateral crura and is often performed in combination with their shortening [4].
Other causes of postrhinoplasty dysfunction of the internal nasal valve: medialization or sliding of triangular cartilages, narrowing of the pyriform opening as a result of an incorrect (pathological) osteotomy line [17].
Uncorrected or residual deformation of the nasal septum.
The septum is the key load-bearing structure of the nose [1]. Its supporting function is not only to maintain the structures of the nose in the desired projection, but also to hold them in the middle position [3]. Deviation of the nasal septum is a fairly common phenomenon; it can be observed in 96.5% of the adult population [14, 18]. In this case, not only the appearance suffers, but also difficulty in nasal breathing.
Often, the close relationship between the deformed external nose and the nasal septum makes it impossible to correct them separately. The deformation of the external nose can be completely eliminated only together with or after correction of the deformed nasal septum.
IN AND. Wojacek (1957) wrote that “...correction of the back without correcting the septum is the same mistake as septum surgery without straightening the back” [19]. H. Vuyk (2000) in his work argued that correction of the bone and cartilaginous pyramid is impossible without mobilization and reposition of the nasal septum [20]. E. Huizing and J. Groot (2003) argued that septal pathology accompanies almost any deformation of the nasal pyramid and spoke of the septum as “the soul of the human nose” [14].
Thus, septoplasty remains one of the most popular operations in rhinology [18, 21, 22].
R. Bracaglia [23] wrote in his work that in 70% of cases, nasal obstruction after rhinoplasty is caused by residual deformation of the nasal septum. M. Constantian [6] even believes that rhinoplasty without correction of the nasal septum is always accompanied by problems with nasal breathing. In turn, submucosal resection of the nasal septum, which is still very popular among ENT surgeons, can subsequently lead to such aesthetic complications as saddle-shaped deformity of varying severity, loss of projection of the nasal tip, retraction of the columella, as well as deviation of the tip and nasal dorsum, secondary violation of nasal breathing [21].
Synechiae of the nasal cavity.
The formation of synechiae in the nasal cavity after rhinoplasty is associated with the intranasal part of the operation. Therefore, their occurrence after rhinoplasty correlates with the frequency of adhesions in the nasal cavity after intranasal surgery and, according to foreign authors, is 2-12%; domestic authors provide data reaching 39% and even 55% [3, 24]. The formation of synechiae after surgical interventions on the external nose, in the nasal cavity and on the paranasal sinuses can nullify the effect of a brilliantly performed operation and return the symptoms of the disease with which the patient consulted the doctor to the starting point. Current methods of dealing with nasal synechiae (washed X-ray film, silicone splints, tubular stents, treatment of “problem” areas of the nasal mucosa with cytostatics, the use of a surgical laser, etc.) do not completely solve this problem. To prevent the appearance of synechiae, according to various authors, an atraumatic operation, prevention of postoperative infectious complications, careful daily postoperative care of the nasal cavity, anemia of its mucous membrane, adequate tamponade and, if necessary, the use of silicone intranasal splints are necessary [20, 25]. Unfortunately, synechiae and cicatricial narrowing of the nasal cavity, being a removable problem, very rarely make a significant contribution to post-rhinoplasty nasal obstruction. More often the problem has other anatomical causes.
Perforation of the nasal septum.
The prevalence of this condition in the population is about 0.9% [26, 27]. Most often, perforations occur after surgical interventions on the nasal septum, when ruptures of mucoperichondrial flaps occur or tissue detachment (preparation) is performed in the submucosal layer, and not between the cartilage and perichondrium. Other iatrogenic factors include transnasal intubation, cryosurgery, cauterization of bleeding vessels on opposite surfaces of the nasal septum, as well as prolonged nasal tamponade. Other known causes: trauma, hematoma or abscess of the nasal septum, exposure to toxic substances, use of cocaine, which has a powerful vasoconstrictor and thrombotic effect. All these factors reduce the volume of blood flow in the mucous membrane of the nasal septum and lead to disruption of trophic processes in the thickness of the cartilage [21, 27].
Perforations of the nasal septum after rhinoplasty can be a consequence of their one-stage correction, too tight and prolonged tamponade, as well as a violation of tissue trophism due to deterioration of blood supply after incisions and rhinoplasty approaches.
The question of the influence of surgical technique on the incidence of perforations remains open at the moment.
Unresolved or newly emerging hypertrophy of the nasal turbinates.
One of the main causes of difficulty in nasal breathing is the pathology of the inferior turbinates, which play a critical role in the implementation of the nasal cycle [1].
The turbinates are represented by bilateral outgrowths of the lateral wall of the nasal cavity and consist of a highly vascularized mucoperiosteum covering a thin semicircular bone. In combination with the internal nasal valve, the anterior end of the inferior turbinate is responsible for 2/3 of nasal airway resistance. Posteriorly, the inferior turbinates diverge from the nasal septum, which reduces respiratory resistance in this area [1, 14].
Otorhinolaryngologists perform a huge number of different operations aimed at reducing the inferior turbinates [14], our review does not aim to describe all of these techniques. Plastic surgeons also often work on the turbinates. Thus, according to N. Tanna et al. [28], members of the American Association of Plastic Surgeons perform the following interventions on the inferior turbinates: lateroposition (49.1%), partial conchotomy (33.3%), radio wave reduction (25.3%), submucosal inferior osteoconchotomy (23.6). %) and electrocoagulation (22.5%). Less than 10% of respondents reported using new technologies such as radiofrequency thermal ablation (5.6%), microdebrider (2.2%), laser photocoagulation (1.1%), or cryosurgery (0.6%). Most often, inferior conchoplasty with lateropexy or submucosal osteoconchotomy of the inferior turbinates is sufficient to achieve good nasal breathing [28]. Aggressive surgical intervention of the inferior turbinates may be complicated by bleeding, dryness and crusting, mucociliary dysfunction, chronic infections, foul nasal discharge, or atrophic rhinitis.
Excessive resection of the anterior end of the inferior turbinates leads to disruption of the nasal cycle, which, in turn, causes subjective difficulty in nasal breathing [1]. At the same time, there remains a huge number of patients with repeated hypertrophy of the inferior turbinates after surgical interventions [14].
In general, from the point of view of the pathogenesis of functional postrhinoplasty problems, it does not seem very correct to expand the cross-section of the nasal cavity, narrowed due to other anatomical formations, by means of correction of the nasal turbinates. The precise role of conchoplasty in relation to rhinoplasty remains to be assessed and requires comparative studies.
There are few published data on the effects of rhinoplasty on olfactory function.
According to the literature, hyposmia after rhinoplasty is in most cases temporary and caused by swelling of the mucous membrane. Permanent anosmia is rare. It is believed that in the 1st postoperative week, 87.5% of all patients after rhinoplasty have anosmia. Elimination of these postoperative phenomena requires a period of 6 weeks to 6 months, after which the sense of smell is supposedly completely restored [29, 30]. Thus, R. Champion [29] observed the state of smell after rhinoplasty in 200 patients, of which only 10 noted subjective anosmia, which disappeared 6–18 weeks after surgery. N. Shamshadi et al. [31] examined 40 patients before and after open rhinoplasty and found that on the 1st postoperative week anosmia was detected in 87.5% of cases; on the 6th postoperative week, 85% of patients had mild to moderate hyposmia and At the 6th postoperative month, the values of olfactory function were identical to the preoperative ones.
C. Kimmelman [32] assessed the olfactory function in 93 patients before and after nasal surgery (including after ethmoidotomy, polypotomy, Caldwell-Luc surgery on the maxillary sinuses, repositioning of the nasal bones and rhinoseptoplasty); in 61 patients, an improvement in the sense of smell was noted, 32 had a decrease. The author found no correlation with age, gender, type of surgery or anesthesia.
The state of mucociliary transport in patients who underwent aesthetic rhinoplasty.
The cause of dysfunction of the nasal mucosa is usually air pollution with harmful substances, gases, dust particles and smoke. Cold air in winter also helps to reduce local immunological resistance and the cleansing ability of the ciliated epithelium of the respiratory tract. Excessively dry or humid hot air leads to a block in the activity of the cilia, which, beating with the same frequency, cannot budge the surface layer of the secretion, which acquires the viscosity of periciliary fluid. The presence of anatomical disorders in the nasal cavity, anomalies of bronchopulmonary structures or congenital pathology of the ciliated epithelium also causes a delay in the evacuation of mucus [1-3]. Any surgical intervention in the nasal cavity and paranasal sinuses affects the effective functioning of the mucociliary apparatus of the nasal mucosa.
Theoretically, surgery on the external nose and intranasal structures may cause dysfunction of the ciliated epithelium. However, in the available literature we have not found any data on the possible effect of rhinoplasty on the transport function of the nasal mucosa.
It is known that patients after rhinoplasty quite often note disturbances in the sensitivity of the tip of the nose and columella [33, 34]. Sensitivity is a person’s ability to sense the impact of various exogenous and endogenous stimuli on his receptor apparatus [35]. It is customary to distinguish between simple and complex types of sensitivity. Superficial sensitivity - the ability to sense irritation of superficial tissues (skin, mucous membranes). This includes pain, tactile and temperature sensitivity [35].
S. Bafaqeeh and M. al-Qattan [33] conducted a study that included 25 patients who underwent open rhinoplasty with a transcolumellar incision using monofilament sutures of varying thicknesses 3 weeks and 1 year after surgery. At the first visit, all patients noted a decrease in the sensitivity of the skin of the external nose in the innervation zones of the external nose. However, 1 year after surgery, most patients experienced complete restoration of sensitivity. And in a study by A. Thompson [34], 65.3% of patients after rhinoplasty noted a decrease in sensitivity of the tip of the nose, in 68.3% of them numbness lasted more than 3 months. Thus, the author concludes that rhinoplasty, accompanied by correction of the tip of the nose, can lead to disruption of its sensitivity.
In order to understand the causes of numbness of the tip of the nose, you need to remember the sensitive innervation of the external nose, which is carried out mainly by the orbital ( n. ophtalmicus
) and maxillary (
n. maxillaris
) branches of the trigeminal nerve.
The supratrochlearis nerve ( n. supratrochlearis
) arises from the first branch of the orbital nerve, the frontal nerve (
n. frontalis
) and innervates the root of the nose.
The subtrochlear nerve ( n. infratrochlerais
) originates from the third branch of the ophthalmic nerve, the nasociliary nerve (
n. nasociliaris
) and, connecting with the supratrochlear nerve, is also involved in the innervation of the external nose.
The anterior ethmoidal branch ( n. ethmoidalis anterior
) also departs from the branch of the ophthalmic nerve (nasociliary nerve) and gives off the final branch - the external nasal nerve (
n. externus nasalis
).
The nerve innervates the distal dorsum of the nose, its tip and the skin of the wings. This nerve appears between the nasal bone and the triangular (superior lateral) cartilages, accompanying the artery of the same name at a distance of 6.5-8.5 mm from the midline and has a diameter of about 0.35 mm. When making an intercartilaginous incision during rhinoplasty, the external nasal nerve is almost always damaged, which causes numbness of the tip of the nose. To prevent this complication, the surgeon should limit the extent of endonasal intervention as much as possible and separate the tissues, moving directly along the surface of the upper lateral cartilage at a distance of no more than 6.5 mm from the midline [36]. anterior superior
alveolar nerve is a branch of the inferior orbital nerve that arises from it even before it enters the inferior orbital foramen. It innervates a small part of the tip of the nose and the columella [36].
Thus, it seems extremely important to use in practical work such techniques that help surgeons preserve the basic functions of the nose during rhinoplasty, and if a problem has already arisen, restore the normal physiology of the nose. Postoperative nasal breathing disturbance should be considered as a complication, the prevention of which is also important as preventing wound suppuration [4].
Realizing that any surgical action that destroys the cartilaginous vault of the nose inevitably narrows the nasal valve, modern surgeons strive to operate as sparingly as possible. This is realized using incisions aimed at preserving the integumentary and soft tissues; resection of only the redundant part of the upper lateral cartilages; suture correction of the tip of the nose; preventing the intersection of domes; maximum preservation of the caudal edge of the nasal septum; resection of the nasal spine only for strict indications; performing medial osteotomy only in exceptional cases [5].
A modern rhinosurgeon is obliged to use such elements of the operation that help reduce the negative functional consequences of rhinoplasty, for example, restoration of the destroyed cartilaginous vault of the nose as a result of removal of the hump. First of all, these are various options for expanding the angle of the nasal valve, among which, historically, spreading dorsal grafts (spreader graft) between the upper edges of the triangular cartilages and the cartilage of the nasal septum have been of leading importance [6]. As the technology was improved, several alternative surgical options were proposed, including the use of a “splay” graft according to B. Guyuron et al. [8], as well as expanding flaps (autospreader flap) [37, 38].
There are other elements of “structure preservation” in rhinoplasty, such as minimizing resection of the lateral crus of the alar cartilages. The correct osteotomy line is of no small importance. The priority for preserving the width of the nasal cavity is percutaneous lateral microosteotomy [8, 14, 39]. The level at which the osteotomy begins should be above the attachment point of the inferior turbinate to the lateral wall of the nasal cavity. Otherwise, as the bones of the nasal pyramid come closer together, the conchae move toward the septum and the nasal passages narrow [39].
The intercartilaginous incision should be made in the groove between the lower and upper lateral cartilages, and not along the edge of the latter, demonstrating sparing treatment of the scroll zone of the triangular cartilages [5]. All incisions of the mucous membrane must be carefully sutured so that there is no excess tissue protruding into the nasal cavity. Otherwise, gross excess scarring may narrow this important functional area [20, 38].
Unfortunately, the nature and severity of the deformation of the external nose in many cases forces the surgeon to perform destructive stages of the operation and ignore the above “structure-preserving” techniques. Otherwise, you simply may not get the desired aesthetic result of the operation, which is the main goal of the intervention.
There is no conflict of interest
.
Author contributions:
Concept and design: I.S.
Collection and processing of material: L.K., E.M.
Text writing: L.K., Yu.R.
Editing: Yu.R.