Rhinoplasty is a complex operation, but it is very popular among patients. Like any other surgical intervention, it has a rehabilitation period with a number of nuances, as well as restrictions and recommendations that must be carefully followed in order to achieve an ideal aesthetic result. As after other types of plastic corrections, swelling of the nose after open rhinoplasty is completely normal. Conservation rhinoplasty does not cause complications such as bruising or swelling.
In fact, no plastic surgery can do without this consequence. Swelling is a natural accompaniment of many interventions. And, of course, such a complex correction cannot but leave traces in the form of swollen tissue. There is no need to be afraid or consider them a complication. The patient’s task is to accelerate tissue healing and relieve swelling. To do this, you must follow your doctor's recommendations.
Why does the nose swell after rhinoplasty?
Any surgical intervention, even the most minimal, is accompanied by damage to tissues and blood vessels. During nose job surgery, the plastic surgeon makes incisions inside the nose itself, peels away tissue to reshape the tip, and so on. This also damages the nasal tissues and capillaries.
After the operation is completed, the injured areas are filled with fluid, which is required so that the tissues regenerate and return to normal as quickly as possible. This is a normal, natural physiological process. While healing is ongoing, swelling after rhinoplasty persists. After the damage heals, new tissues form and blood circulation improves in the operated area, the fluid will go away, and along with it the swelling will go away.
Variant of the norm
Full recovery after rhinoplasty takes time. Formation of the final contours of the nose takes 12-18 months. Therefore, if less than 6 months have passed since the operation, then it is too early to talk about any complications of rhinoplasty.
During the rehabilitation period, the tip of the nose may look slightly upturned or, conversely, drooped. We understand that you would like to see the results you dreamed of sooner. Be patient.
Tissue swelling persists for 2-3 months after rhinoplasty. Gradually it will subside, the swelling will go away, the nose will look somewhat thinner, more graceful, its length will visually decrease, and its tip will change its position.
How far can he go?
On average, the tip of the nose drops by 3 mm within six months. This is not a surgical defect, but a natural phenomenon when tissues take root in a new position and the consequences of rhinoplasty disappear.
If you are unsure whether your rehabilitation is proceeding correctly, contact your plastic surgeon. Knowing all the specifics of your case, he will explain what results you should expect.
How long does it take for swelling to go down after rhinoplasty?
Conventionally, the rehabilitation period can be divided into several stages. The first period begins immediately after surgery. Tissue swelling forms immediately after the intervention and continues to grow over several days. Swelling after surgery reaches its maximum peak approximately on the third day after correction. At first, tissue swelling will be noticeable not only on the nose, but also on the chin and cheeks.
It is important to note that the formation of bruising and swelling is directly related to the type of correction performed. After closed (conserving) rhinoplasty, there is no swelling or bruising, and the patient can return to normal life the very next day after surgery.
Nose surgery helps achieve ideal aesthetics. Before and after open conservation rhinoseptoplasty.
With open or regular correction, already in about the third week, discomfort and unpleasant sensations decrease and pain goes away. Swelling and bruising gradually decrease, but secondary swelling remains. It is often virtually invisible to the patient. After two to three months, the visible swelling after correction completely disappears. But it is impossible to talk about the complete disappearance of puffiness. In general, if we talk about the average time frame for swelling to subside after rhinoplasty, then it goes away from the root of the nose in 2-3 months, from the back in 4-6 months, from the tip in a year and a half.
Is it painful to remove the cast after rhinoplasty?
After rhinoplasty, after a week or 10 days, the plaster cast or special nasal splint is removed. By this time, the initial severe swelling has already partially subsided, the bandage does not lie so tightly and dangles. Therefore, removing the plaster is almost painless. In rare cases, it flies off on its own.
See also our separate article “How many days is the cast removed after rhinoplasty?”
Important! It is strictly forbidden to remove plaster yourself. Otherwise, this will lead to unwanted complications.
When will it be possible to return to normal life?
Having learned when swelling goes down after rhinoplasty, some patients become tense, thinking that after surgery they will have to walk with swelling for a year. This is wrong. The swelling, clearly visible to the naked eye, goes away after the usual correction within three weeks after the intervention. After a month, the nose acquires a neat, even shape and aesthetic appearance. With the preservation technique, due to the absence of postoperative traces, the aesthetics are not compromised at all.
Over the course of a year and a half, there is a gradual decrease in size. And after this period we can already talk about the final aesthetic result and its consolidation. It is at this time that the surgeon and the patient can sum up the final results of the correction. Therefore, if you hear as an answer to the question how long swelling after rhinoplasty lasts, about a year or more, you should not worry.
Rhinoplasty for deviated nasal septum
Rhinoplasty as a technique for correcting congenital or acquired deformities of the nose has been practiced since ancient times. Over time, nose surgery has become one of the complex areas of plastic surgery, responsible not only for aesthetics, but also for the functions of the most important human respiratory organ. Operating otolaryngologist, rhinoplasty surgeon at the Scandinavia clinic, Evgeniy Valentinovich Sharin, spoke about how broad the goals of modern rhinoplasty are, and why not every patient has access to the nose of his dreams.
Sharin Evgeniy Valentinovich Otorhinolaryngologist
Rhinoplasty as a technique for correcting congenital or acquired deformities of the nose has been practiced since ancient times. Over time, nose surgery has become one of the complex areas of plastic surgery, responsible not only for aesthetics, but also for the functions of the most important human respiratory organ. Operating otolaryngologist, rhinoplasty surgeon at the Scandinavia clinic, Evgeniy Valentinovich Sharin, spoke about how broad the goals of modern rhinoplasty are, and why not every patient has access to the nose of his dreams.
– Let’s be clear, is rhinoplasty still a field of aesthetic medicine?
– Rhinoplasty is one of the components of aesthetic medicine, but at the Scandinavia clinic we provide it because all plastic surgeries on the nose are functional. For a patient, a “beautiful” nose is one that meets some of his worldview characteristics. For a doctor, the nose should not only be attractive in appearance, but also function correctly as an organ - perform respiratory, resonator, and olfactory functions. You can remove the hump and at the same time narrow the nose so that the patient returns after some time with breathing problems. Today, all surgeons performing rhinoplasty follow the principle that any nose can be made “beautiful” within certain limits.
– Let’s imagine that a patient comes to you who wants to have a nose job. What happens next?
– I repeat that most often people come to our clinic with functional disorders. It happens that a patient needs to restore nasal breathing, but the shape of the nose can also be adjusted according to his wishes: reduce or enlarge, remove a hump, or a deviated nasal septum. The patient’s wishes must be strictly defined - demands such as “make me beautiful” are mostly impossible to fulfill.
Any modern plastic surgery is preceded by computer modeling, when we imagine the face in certain projections and work out the shape of the nose in accordance with the wishes of the patient and surgical principles. Next, the patient is sent for examinations - computed tomography, blood tests, consultation with a therapist, and after that the date of the operation is determined. On the appointed day, the patient comes, talks with the anesthesiologist (rhinoplasty is performed under general anesthesia) and signs the necessary documents.
The operation itself and recovery after it can take different times depending on what manipulations we perform. Typically, the operation lasts from 2 to 3.5 hours. Within a week, swelling decreases, and stitches and plaster (if required) are usually removed after 10-12 days. The sutures inside the nose dissolve on their own within 3-4 weeks. The nose takes its final shape 6 months after surgery in the case of primary rhinoplasty. With secondary rhinoplasty, this may require 1-1.5 years, but changes in such a long-term period are, as a rule, insignificant.
– What methods of rhinoplasty exist?
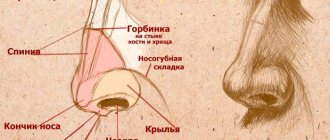
– Rhinoplasty is performed using open and closed access. In the first case, a skin incision is made in the area of the septum (columella), and the skin is separated from the cartilaginous and bony framework of the nose. Closed - everything is the same, only all the incisions are made inside the nasal cavity. With the closed method, the neurovascular bundle of the columella is not intersected, so the recovery period is faster, but in general the difference is insignificant. Today, surgeons vary these methods because the approach to each nose is individual. There are no two identical operations, and there are no clear supporters of one method or another.
– There is a fairly long list of contraindications for rhinoplasty. From the completely understandable (blood diseases, oncology, diabetes) to the unobvious such as mental disorders... What other restrictions should be taken into account?
– An important limitation is also the age of the patient. Until the age of 18, when the nose is not yet fully formed, plastic surgery, both internally and externally, is not performed. After 50, natural tissue withering begins, and again the result is unpredictable.
– Everyone’s nose is different, and probably not every nose can be made beautiful?
– The doctor’s conclusion is not limited to the definition of a “beautiful” or “ugly” nose. The concept of a “beautiful nose” is subjective, expressing only an aesthetic, secondary function from a biological point of view. It is always possible to identify anatomical changes that do not fit into the standard characteristics: humps, deviated nasal septum, scoliosis, recessed nasal dorsum - all this requires correction, because it is not only noticeable, but also affects the intranasal structures. The surgeon’s task is to explain to the patient that, from the point of view of modern rhinoplasty surgery, a beautiful nose is a well-breathing nose that meets beauty standards and that the patient himself likes. Therefore, it is necessary to explain the close connection between the anatomy of the nose and its functions, and to show the negative effect of a sharp narrowing of the external nose on nasal breathing. Rhinoplasty is a very complex operation that requires jewelry work. But despite this, 100% implementation of the plans of the surgeon and the patient is impossible. An adequate person, of course, will listen to the words of a specialist, if he is not an enemy to his health. If the patient is categorically against it and, despite the arguments given, insists on his own, then no contact is built and, as a rule, we part.
– Does it happen that patients are dissatisfied with the result of a plastic surgeon’s intervention?
– Yes, but, fortunately, this does not happen often. In such cases, if possible, repeat corrective surgery is performed. It is important to understand that after surgery, the shape of the nose will never be 100% consistent with what was modeled on the computer, because some tissue healing processes cannot be completely controlled. It is especially difficult to satisfy all the patient’s requirements when the aesthetic component is brought to the fore - and this happens in any clinic. Nose operations are, without exaggeration, the most difficult in plastic surgery.
– It is obvious that the shape of the nose carries something more than just anatomical features, do you agree with this?
– The nose is truly an “outstanding” facial structure in every sense that catches the eye first. The patient may have a strong complex if his nose has an irregular shape, and this affects his quality of life, he is depressed by this condition, and his social adaptation is difficult. With the help of rhinoplasty, a person can forever get rid of the complex associated with the shape of his own nose. Therefore, for many patients, surgery to correct the shape of the nose is the starting point of a new life, so to speak.
How to reduce swelling after rhinoplasty?
To alleviate their condition and speed up rehabilitation, the patient must follow the recommendations. For example, correcting your diet will help relieve swelling after rhinoplasty, in particular avoiding salt and spicy seasonings, which retain moisture in the body. Immediately after surgery, it is better to sleep in a semi-sitting position. You should not visit baths, saunas, or take a hot bath to prevent blood flow to the operated area. A cold compress is recommended on the injured area.
The swelling goes away quite quickly: within a few months you can make the first assessment of the new shape and size of the nose.
It is also strongly recommended to reduce physical activity, especially avoid movements that require bending the head or body forward. And it is very advisable to eliminate bad habits during recovery - drinking alcoholic beverages and cigarettes. By following these simple rules, you can quickly remove swelling after removing the rhinoplasty cast.
Treatment options
To prevent the proliferation of connective tissue, treatment is prescribed immediately after rhinoplasty, if it was performed with osteotomy, that is, excision of part of the bone. In case of excessive callus formation, a combined treatment method is used, including medications and physiotherapeutic procedures. If the measures taken do not help, then the issue of repeated surgical intervention is decided.
Drug treatment
To reduce swelling and prevent wound infection, relieve the inflammatory reaction, decongestants and antibiotics are prescribed.
If the callus has grown excessively, a number of medications are additionally prescribed:
- injection of hormones, primarily hydrocortisone, which relieves inflammation and helps soften calluses;
- drugs that have a catabolic effect on connective tissue, that is, they help to reduce it;
- ointments with steroid hormones on the area of nose correction.
Additionally, general strengthening agents are prescribed, such as vitamins, painkillers and medications to normalize scarring.
Physiotherapy
Physiotherapeutic procedures contribute to the resorption of callus. The main methods used to remove growth:
- Magnetotherapy is the effect of magnetic fields on bone formation. A static magnetic field improves metabolic processes, stimulates the immune system and is used as an auxiliary method for removing calluses.
- UHF - ultra-high frequency electromagnetic oscillations enhance blood microcirculation, promote the flow of substances necessary for resorption into the inert callus, and enhance metabolic processes in bone formations.
- Ultraphonophoresis is a method of physiotherapy that combines ultrasonic vibrations with the effects of medications. By improving metabolic processes, ultrasound, when applied locally, ensures the delivery of drugs to the bone growth. A steroid ointment, usually containing lidase and hydrocortisone, is used and applied to the surface of the skin. Steroids help soften bone, and ultrasound increases the permeability of the skin and other tissues, reduces the sensitivity of nerve endings, and regulates the activity of the peripheral nervous system.
Revision rhinoplasty
A radical method such as revision rhinoplasty is prescribed in cases where drug therapy has not given the desired result. The operation allows you to remove callus and restore the aesthetics of the nose. It is prescribed after final recovery, which lasts a year, and drug treatment, which takes another year. A noticeable aesthetic defect becomes an indication for revision rhinoplasty. After additional diagnostics, a surgical plan is developed and the callus is excised.
Drug treatment
If the patient has a slight increase in body temperature, antibacterial treatment may be prescribed. Painkillers are prescribed to relieve pain. If there is a lot of swelling after rhinoplasty, the doctor may prescribe special gels or ointments that help resolve the swelling and bruises at the correction site. For example, “Traumel” or “Badyaga”. You can also rinse your nose with saline solutions based on sea water.
How to remove swelling after rhinoplasty using medication, what ointments to use - all this should be discussed exclusively by a surgeon, since each treatment is individual. Do not use medications without first consulting your surgeon!
Reasons for education
During the rhinoplasty process, some elements of the nasal structures are removed or damaged. For example, if a bone was injured during rhinoplasty, our body activates a protective mechanism and begins to form a growth at the site of tissue damage.
Formation consists of three stages:
1. Formation of a provisional callus;
2. Appearance of osteoid tissue;
3. Replacement of connective tissue fibers with bone ones.
But there are incidents where initially cartilage appears, which transforms into bone.
Callus is also divided into three types:
- Periosteal - external, formed from the outside, where the periosteum is;
- Endosteal – internal, formed in the bone marrow cavity;
- Intermediate – intermediate, formed between external and internal.
Most often, callus occurs in 17-18 year olds because the bones and cartilage are still developing. For this reason, rhinoplasty is recommended after the age of 25, when development is complete.
Photos from open sources
When should you worry?
If swelling after rhinoplasty does not go away within the time frame specified by the doctor, this is not always a sufficient reason to start panicking. The fact is that the period of resorption of swelling is individual for each patient. Just following the recommendations is not enough; the rate of tissue healing is largely determined by innate parameters. Thus, some patients have longer recovery times and some have shorter ones.
But there are also situations like this:
- regeneration was noticeably delayed,
- swelling does not lose its severity for a long time,
- the operated area is painful on palpation,
- there is suppuration or heavy bleeding,
- body temperature is very elevated for several days.
These and other situations where unusual sensations, increased discomfort or other uncharacteristic phenomena occur require immediate contact with your doctor.
Clinical case
A patient with AE came to the Institute of Plastic Surgery and Cosmetology (IPCC) after undergoing injection rhinoplasty with a filler based on HAP. Main complaints: swelling, pain and redness of the back and tip of the nose after the procedure (Fig. 1).
Rice. 1. Self-photo of the patient 5 hours after the injection rhinoplasty procedure.
On examination: moderate swelling, redness and tenderness of the dorsum and wings of the nose (Fig. 2).
Rice. 2. Clinical picture when visiting the IPC on the 3rd day after the injection of a filler based on HAP into the area of the back and tip of the nose. On palpation: pain and tissue tension without local areas of compaction.
From the anamnesis: 3 days ago, at a medical institution, a cosmetologist performed a procedure for correcting the back and tip of the nose with a filler based on HAP microparticles registered in the Russian Federation. The drug was injected subcutaneously into the area of the nasal dorsum with a 25G cannula, and into the area of the tip of the nose with a needle. The total volume of the administered drug was 0.35 ml: 0.3 ml - into the back of the nose, 0.05 ml - into the tip of the nose. The procedure and the immediate post-procedural period were uneventful.
5 hours after the procedure, the patient noted the appearance of severe pain and redness of the tip and dorsum of the nose. A day later, pronounced swelling began. The attending physician prescribed: dexamethasone 4 mg and suprastin 1 ml intramuscularly to relieve swelling (once), orally - aspirin 75 mg (improving the rheological properties of blood), sildenafil (vasodilatation and improving tissue trophism), nurofen (relief of inflammation). Over the next 2 days the picture did not change significantly.
An ultrasound examination (US) performed at the IPC revealed moderate swelling of the soft tissues of the nose. During ultrasound Doppler examination, the vascular pattern in the superficial tissues of the nose was not determined.
At the consultation, the question was raised about the interpretation of examination data, assessment of clinical dynamics and ultrasound results for making a diagnosis and prescribing adequate treatment.
The first diagnostic hypothesis was associated with the introduction of the drug into the lumen of the superficial artery of the dorsum of the nose. An aspiration test was not performed by a physician, and the use of a needle presented an additional risk when correcting problem areas in terms of possible vascular perforation. However, during the procedure and immediately after it, phenomena characteristic of arterial embolism such as severe pain, whitening of tissue, and subsequently the development of a livedo pattern were not observed [3]. However, according to C. De Lorenzi [3], skin whitening is not a pathognomic symptom of vascular occlusion and can be so short-lived that the doctor does not attach any importance to it. It is possible that the introduction of a minimal volume of heterogeneous material into the nasal artery did not lead to its occlusion and was accompanied by the movement of particles upward with the blood flow, followed by occlusion of smaller vessels - arterioles and precapillaries. Therefore, the observed clinical picture was more typical of capillaropathy. Moreover, according to the Doppler study, there was a lack of superficial blood flow.
The second version was possible compression of the nasal vein by the injected filler. It is important to note that over the previous 2 months, the patient had the back and tip of her nose corrected twice with the same drug. The doctor deliberately used a step-by-step correction tactic, avoiding the immediate injection of a large volume of filler into the corrected area. The mechanism of action of the material based on HAP microparticles is associated with the stimulation of collagen synthesis and the formation of a perifocal focus of fibroplasia [4], which in this case could lead to a limitation of the initially small capacity of the soft tissues, to the development of compression of the nasal vein by the injected drug with subsequent stagnation in the form of hyperemia , pain and swelling. The manifestation of the consequences of venous compression 5 hours after the procedure may be explained by additional complications in the form of increasing edema. Venous embolism is unlikely, since in the case of a superficially located vessel, the clinical picture of complete occlusion would be somewhat different.
It should be emphasized that there was no evidence of an infectious process.
The situation with the impossibility of promptly clarifying the diagnosis, on the one hand, and the need for active treatment of presumably compression-ischemic disorders, on the other, confronted doctors with the need to include nonspecific effects in the complex of therapy, allowing them to overcome possible tissue hypoxia (hypothesis 1) and “unload” the tissue space around the introduced material (hypothesis 2), as well as carry out preventive sanitation of the problem area.
The patient was given a single intramuscular injection of dexamethasone 8 mg, it was decided to continue taking aspirin 75 mg/day daily (the patient took it for 1 week), and the problem area was injected with 0.7 cm3 of an oxygen-ozone mixture.
As evidenced by our own experience and literature data [5, 6], ozone therapy has anti-inflammatory, bactericidal, analgesic, immunomodulatory, detoxifying effects, and helps improve microcirculation. Moreover, the oxygen-ozone mixture activates catabolic, including redox processes in tissues, saturates the blood with oxygen, and has an antihypoxic effect [7], which in general fully corresponded to the stated therapeutic objectives.
Injections of the oxygen-ozone mixture were accompanied by painful sensations, but the color of the skin immediately changed - the cyanotic tint disappeared. After half an hour of observation, the patient was sent home. Over the next 2 days, the patient received injections of an oxygen-ozone mixture. After 3 ozone therapy procedures, swelling and pain resolved, the color of the skin of the tip of the nose was almost equal in color to the surrounding healthy skin. At a follow-up visit 1 month after treatment, complete restoration of the skin of the nose was noted (Fig. 3).
Rice. 3. Dynamics after 1 month.