Many people are terrified of anesthesia. Sometimes this fear is based on terrible rumors, and sometimes it is not based on anything. There is just such an irrational fear.
In fact, the patient’s chance of dying “from anesthesia” is much less than the chance of sudden death in his sleep in his own bed (according to statistics - 1 case in 250 thousand operations). Most accidents and complications from anesthesia occur during major, emergency and very long surgeries. They do not exist in plastic surgery, just as there are no patients with severe cardiac pathologies and no urgent operations for patients in serious condition. So the risk is almost zero. But accidents happen, right? According to the Ministry of Health, they do happen, but, I repeat, very, very rarely.
What kind of anesthesia is there?
Modern anesthesia is multicomponent. We use not one, but several different drugs at once. Some provide complete pain relief, others provide medicated sleep, and others provide muscle relaxation.
There are also several ways to deliver drugs into the body:
- combined (multicomponent) anesthesia.
- intravenous anesthesia;
- inhalation anesthesia;
- combined anesthesia
- spinal and epidural anesthesia;
- local anesthesia;
For each type of operation, we select the optimal combination of drugs and the method of their use in order to achieve the full effect using lower doses of medications and eliminate possible complications.
Methods of carrying out
Depending on the method of correction, there are:
- Open method.
- Closed method.
- Non-surgical correction.
Based on the direction, correction of the shape of the nose is divided into the following types:
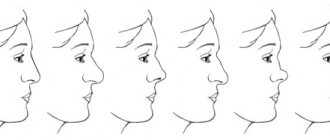
- Aesthetic rhinoplasty - involves correcting the shape and location of the nasal cartilage at the tip, narrowing and correcting the shape of the wings, eliminating nasal humpback. The operation time is up to 2 hours.
- Reconstructive rhinoplasty is performed with the introduction of implants (correctors), transplantation of cartilage tissue and soft tissue mass. Duration – 2-6 hours.
Method without surgery
Non-surgical correction is carried out with injections of hyaluronic acid, collagen and synthetic polymers. It is performed more often without additional anesthesia. It differs from surgical correction methods in its temporary effect. If necessary, topical painkillers (ointments, gels) can be used.
Non-surgical methods also include the use of dermatological fillers and special threads (threads are implanted through small holes and the desired nasal areas are tightened). The manipulation is performed under local anesthesia.
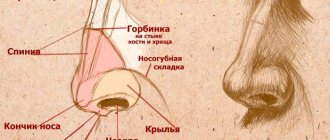
Open method
This method of surgical intervention provides the doctor with wide access to the operated area. The area of the surgical field depends on the specifics of the intervention.
Features of the technique include:
- The incision is made at the column of the nose or at the base of the nostrils.
- The dermis is retracted upward, and the cartilaginous and soft tissues are separated.
- If necessary, the cartilaginous hump is cut off.
- The lid of the nose is closed by lateral displacement of the bones.
- The tip lock is installed.
- The tip is tapered by stitching together pieces of cartilage.
- The dermis is lowered and fixed.
- Stitches and special splints are applied.
The surgery is performed under general anesthesia and lasts from 30 minutes to 2 hours.
With an open technique, it is permissible to use a laser to make the cut. The laser cut is smooth and precise, and it also promotes simultaneous blood coagulation.
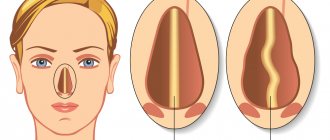
Closed method
A closed operation is carried out in several stages:
- A small incision is made in the mucosal area. Several access methods are possible: marginal access (through the nostril edge), through cartilage, transfection access.
- Correction of tip deformation.
- Stitching.
The operation time is from half an hour to 40-45 minutes. The advantage of the closed technique is that the seam is invisible (the incision size is about 5 millimeters).
The disadvantages of this method include:
- the surgeon is limited in his actions due to the small size of the surgical field;
- inability to control vascular damage (risk of hematomas and blood clots).
Features of general anesthesia in plastic surgery
In plastic surgery the following is used:
- Combined multicomponent anesthesia is the sequential or simultaneous use of various anesthetics, as well as their combination with other drugs. This method allows us to obtain the triple effect we need: pain relief, sedation and muscle relaxation while simultaneously reducing the concentration (or dose) of the anesthetics used.
- Combined anesthesia is anesthesia when the patient’s consciousness is turned off by a general anesthetic during the operation, and peripheral analgesia and blockade of the autonomic nerves are provided by one of the local anesthetics. At the same time, it is possible to significantly reduce the effective doses of the drugs used, which means the risk of complications is significantly reduced.
Why don't plastic surgeons like local anesthesia?
Most experienced plastic surgeons, even when performing minor aesthetic corrections (for example, blepharoplasty), recommend their patients general rather than local anesthesia. There are reasons for this. One of them is quite obvious - both the surgeon and the patient are more comfortable when the subject of the operation is quietly sleeping and does not disturb the doctor with questions: “What did you just cut off from me?” And the second reason is that the introduction of local anesthetics directly into the correction area distorts the relief (configuration) of the surgical field, which may prevent the surgeon from correctly assessing its parameters and affect the final result of the operation.
However, this is not the only reason to choose general anesthesia rather than local anesthesia. The fact is that in addition to painlessness, other conditions are needed for the success of the operation: firstly, optimal blood pressure, and secondly, muscle relaxation. Both of these parameters are regulated during combined anesthesia.
Rhinoplasty is a serious and quite time-consuming plastic surgery. Naturally, during a consultation with a plastic surgeon, the future patient discusses in detail all the details of the upcoming intervention.
At this point, the surgeon devotes a lot of time to removing fears and prejudices associated with anesthesia. Questions can range from the most naive, for example, “how will the nose breathe during surgery?”, to quite professional ones, such as “will endotracheal anesthesia be used?”
It is clear that such issues will be resolved by a council of doctors, and the final word will belong to the anesthesiologist-resuscitator.
But there are general rules that all clinics follow, which guarantee high quality medical care - anesthesia for rhinoplasty must be justified according to the indications, the method of intervention, and be safe.
But often the patient is worried, afraid of general anesthesia and persuades the doctor to perform rhinoplasty under local anesthesia.
Where do these fears come from? From those memorable times when operations were performed without anesthesia at all, or the patients were killed on the spot with ether and chloroform, like Nikulin’s hero in “The Extraordinary Adventures of Shurik.” Remember, I trained on cats!
The task of that outdated type of anesthesia was one - to switch off the patient. And it doesn’t matter in what way! After all, once upon a time the patient was given only a glass of vodka and then was wielded with metal instruments for a long time.
Today, anesthesiological assistance is an accurate and humane medical science that correctly calculates its strength in the fight against pain. Her latest achievement was medical sleep, which “turns off” the patient’s consciousness without causing harm to the body.
If a plastic surgery clinic considers its advantage that rhinoplasty surgery is performed under local anesthesia, this indicates two equally dangerous things for the patient:
Firstly, the clinic probably does not have modern anesthesiological equipment or equipment that would monitor the state of the body during surgery. There is also no experienced anesthesiologist-resuscitator on staff who provides professional anesthesia.
Rhinoplasty under local anesthesia involves numbing a small area. Yes, the patient does not experience pain, but he sees and hears everything that happens before his eyes (here is his nose, next to him!).
And this is actually a great stress for the psyche: hearing the sound of an instrument, seeing a flap of skin, prepared from other tissues and hanging in a metal clamp in front of the eyes. And this is the “second thing”: the task of doctors is not to demonstrate their skills to the patient with their eyes wide open, but to carry out the operation while maintaining the patient’s health and mental balance.
For rhinoplasty, of course, only general anesthesia can be used, the safety of which is guaranteed by an anesthesiologist.
The list of equipment that a clinic must have takes up an entire page. A separate room is required for the anesthesia machine. All this is available in those clinics that have received a license for plastic surgery, added an anesthesiologist and a nurse anesthetist to their staff, and ensured a shared understanding of the process among the entire operating team.
During rhinoplasty, the nose, of course, does not breathe on its own: a special tube is inserted into the patient’s trachea, which provides air and prevents blood and mucus from entering the esophagus and lungs.
Since the operation can last from two to four hours (in especially difficult cases), the constant presence of an anesthesiologist-resuscitator ensures monitoring of the patient’s condition: oximetry (measurement of oxygen content in the blood), measurement of blood pressure, respiratory rate, body temperature, An electrocardiogram is taken.
In fact, your health has never been more controlled than with general anesthesia!
To ensure that the pain syndrome does not disturb the sleeping patient, local anesthesia can also be administered at the site of exposure as an additional means of pain relief.
A full-time anesthesiologist-resuscitator is also present when the patient wakes up: he makes sure that everything went well and that the patient feels well.
Further in the medical history, the patient’s condition during and after the operation is described in detail, which allows for proper rehabilitation and restoration of the body in the future.
Plastic surgery, including rhinoplasty, is not the lunchtime office procedure it is sometimes portrayed to be. Therefore, if you are faced with a decision - which clinic to go to, where to get a nose job, choose not the one where they will tell you that they will fulfill all your aesthetic wishes under local anesthesia, but the one in which plastic surgeons and anesthesiologists-resuscitators understand the seriousness of operation and observe all safety measures during its implementation.
Why are pressure levels and muscle relaxation so important?
A plastic surgeon works with soft tissue and skin. Will he be able to do a perfect blepharoplasty if the facial muscles are tense from fear or some involuntary movements suddenly occur? Experienced surgeons say that with general anesthesia, even the elasticity of the skin changes. It is more convenient to work with it, which means it is easier to achieve the desired result.
As for pressure, it must be strictly controlled and in no case increased. Otherwise, bleeding or hematomas may occur, which subsequently lead to the formation of a rough postoperative scar.
Rehabilitation after rhinoplasty
After surgery, the back of the nose is fixed with a plaster cast.
Rehabilitation after rhinoplasty involves complete rest for 1-2 days. The patient is not recommended to get out of bed; in the first weeks, sleeping is allowed only on his back. Severe pain in the nose area can be relieved with painkillers prescribed by the doctor. 1-2 days after nasal tip surgery, the patient can leave the hospital and go home. The plaster cast is removed after 2 weeks; the patient can return to the usual rhythm of life in about 2-3 weeks. The swelling goes away after a month; during this period you should not wear glasses or bother yourself with heavy physical activity. During rehabilitation after rhinoplasty of the tip of the nose.
Hot baths, sunlight, abuse of alcohol and hot drinks, fatty and spicy foods should be avoided. If the patient cannot do without glasses, you should worry about a lighter frame. The final “shrinkage” of the tip of the nose occurs 6-8 months after surgery. Rhinoplasty of the tip of the nose in Moscow is offered by many clinics and medical centers, as well as beauty salons.
Contraindications for the use of general anesthesia
Before plastic surgery, you undergo a full examination, during which we make sure that you have no contraindications to the operation. If you have high blood pressure or some kind of heart problem, this is not always an obstacle to surgery. In each specific case, this issue is discussed in detail after a careful examination by a specialized specialist, taking into account the duration and complexity of the planned intervention, as well as the new possibilities of modern anesthesia.
Contraindications for elective general anesthesia are:
- From the cardiovascular system: acute coronary syndrome or recent (1-6 months) myocardial infarction, unstable angina or exertional angina of functional class 4, congenital or acquired defects of the mitral and aortic valves; disturbances of conduction and rhythm of the heart - atrioventricular block, atrial fibrillation with failure of the contractile function of the heart, increasing chronic heart failure,
- From the respiratory system: bronchial asthma in the acute stage, pneumonia, severe obstructive bronchitis, respiratory failure. ARVI and, as a result, acute laryngitis or tracheitis.
- Kidney and liver diseases: acute liver or renal failure, viral and toxic hepatitis in the acute stage, liver cirrhosis, acute pyelonephritis, acute glomerulonephritis.
- From the nervous system: psychiatric diseases, severe injuries and contusions of the brain (1-6 months).
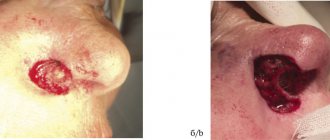
- Foci of infection in the body. If possible, surgery should be postponed until the infection is completely cured. These can be abscesses, cellulitis, erysipelas on the skin.
But in the case of most chronic diseases (not in the acute stage), operations can be performed subject to more thorough preoperative preparation and individual selection of anesthesia drugs.
Contraindications
Rhinoplasty surgery is contraindicated before reaching adulthood - age restriction. Correcting the shape of the nose surgically is prohibited in case of acute chronic diseases and blood coagulation disorders.
The list of contraindications and restrictions also includes:
- inflammatory processes localized both on the external nasal surface and on the mucous membrane of the nostrils;
- During pregnancy and breastfeeding;
- tumor diseases;
- systemic infections;
- liver lesions;
- renal failure;
- diabetes.
Whether a patient can undergo surgery is decided by the surgeon based on tests and medical history, so some restrictions may not be absolute.