Despite the fact that large breasts are the ultimate dream of many representatives of the fair half of humanity, some of their owners have to resort to plastic surgery. A pathology such as gigantomastia is characterized by the growth of the mammary glands to gigantic sizes and their loss of their shape. Reduction plastic surgery for gigantomastia allows a woman to be relieved not only from physical, but also from psychological discomfort. Gigantomastia in women can cause:
- pain in the neck, back, chest;
- occurrence of mastitis;
- development of mastopathy;
Reduction mammoplasty for gigantomastia - RUB 210,000.
Included in the price:
surgery, consultation with an anesthesiologist, anesthesia, hospital stay with meals, dressings.
40-90 minutes
(duration of operation)
5-7 days in hospital
Indications
- gigantomastia
Contraindications
- acute infectious diseases
- chronic diseases in the stage of decompensation
- age up to 18 years
Causes and types
The reasons for the development of gigantomastia lie in genetic predisposition. This means that the pathology is not acquired and can manifest itself at any age. It is customary to distinguish:
- pubertal hypermastia - characterized by the proliferation of glandular tissue and occurs during puberty;
- postpartum hypermastia - characterized by the proliferation of adipose tissue, occurs after childbirth.
One of the reasons for the progression of the pathology is a violation of lipid metabolism. If a woman actively gains weight, then the fatty tissue of her breasts grows in volume.
Stellar giganomastia
Last year, Anna Semenovich admitted to this disease on Lera Kudryavtseva’s show. The public has long been agitated by the question of the performer’s gorgeous bust; everyone wondered who was the “author” of such large breasts, as it turned out - nature. Anna Semenovich's large breasts became more of her punishment than her reward.
The star admitted that her huge bust caused a lot of physical discomfort and was the cause of bullying and a lot of complexes. At a certain point, Anna Semenovich underwent plastic surgery, but she did not enlarge, but reduced her breasts! And her only regret is that she didn’t do it earlier and didn’t agree to an even smaller size.
The before and after photos of Anna Semenovich are strikingly different, as the performer admits, she changed her size 9 to 5 and feels great!
As Anna says, her breasts weighed about 3 kg each and caused a lot of inconvenience, from moral and psychological to purely physical - they interfered with normal sleep, breathing, and caused constant pain in the back and shoulders.
Certain symptoms of macromastia were also observed in Alena Vodonaeva, the star of the “House 2” project. Already at the age of 16, the girl could boast of a full “A”, and after the birth of the child, her breasts became even larger and it is possible that they continued to grow. However, the girl clearly did not like such “generous forms” against the backdrop of general thinness and she decided to have surgery. Alena trusted herself only to American doctors and the result exceeded all expectations. Now the star just has beautiful breasts. Photos before and after Alena Vodonaeva clearly show that the operation is to her benefit.
How is reduction mammoplasty performed at CELT?
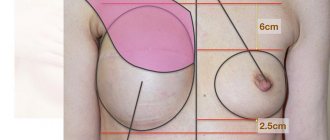
The most effective treatment for gigantomastia is breast reduction surgery. This operation is called reduction mammoplasty. Before proceeding with surgery, the plastic surgeon will apply markings to the patient's skin. Typically, excess tissue is removed in the lower sector of the breast. Reduction mammoplasty is aimed at solving three main problems:
- excision of excess glandular and adipose tissue;
- elevation of the nipple-areolar complex;
- excision of stretched skin.
The operation is performed under general anesthesia and allows:
- significantly reduce breast volume;
- create a beautiful shape of the mammary glands;
- preserve not only the sensitivity of the nipple, but also the possibility of lactation.
At the end of the operation, the surgeon applies invisible cosmetic sutures.
The specialists of the multidisciplinary CELT clinic take full responsibility in preparation before surgery and evaluate a number of parameters and individual indicators of the patient. At the same time, they take into account her wishes regarding the appearance of her breasts.
When large breasts become a symptom of gigantomastia
The size of the bust is a relative concept: what is excessive for a petite girl will be the norm for a stately lady 180 cm tall. You cannot diagnose “hypermastia” only on the basis that a woman is burdened by this natural “wealth”. Excessively large breasts provoke pain in the spine, the formation of bleeding grooves on the shoulders from bra straps and can cause serious psychological disorders due to ridicule and increased “attention” from others. The main symptom indicating hypermastia is intensive breast growth. When the volume of an organ increases over several years or even months. Another symptom that should alert you is a breast weight of more than 2.5 kg .
Shibelgut N.M., Vlasova V.V., Batina N.A., Elgina S.I., Moses V.G., Moses K.B., Rudaeva E.V.
GAUZ Kuzbass Regional Clinical Hospital named after. S.V. Belyaeva, Kemerovo State Medical University, Kemerovo, Russia
GESTATIONAL GIANTOMASTIA (CLINICAL CASE)
Gigantomastia (macromastia, hypermastia) is a rare disease associated with excessive hypertrophy of the connective tissue of the mammary gland in women. Gestational gigantomastia is a type of disease and the most common type. It develops during pregnancy under the influence of hormonal surges of progesterone, prolactin, and estradiol. More often, gigantomastia is bilateral, less often - unilateral. The disease occurs in one case in 28,000-100,000 pregnancies. As a rule, the condition develops in the first trimester of pregnancy under the influence of placental hormones. The consequences of the disease are more often observed in women with multiple pregnancies. Approximately 150 cases of gestational gigantomastia have been reported. After childbirth, in some cases, the breasts return to their postpartum state, but with subsequent pregnancy they increase again, usually more significantly. The condition threatens the health of the mother, but has a good outcome for the fetus. Despite the benign nature of gigantomastia, it can cause a dangerous condition and even death from severe infection and cardiopulmonary failure. This article describes a rare clinical case of gestational gigantomastia. Taking into account the optimal chosen tactics for managing the patient, a relatively favorable outcome was obtained for the woman, pregnancy and childbirth for the mother and fetus.
Keywords:
gestational gigantomastia; pregnancy; childbirth
Shibelgut NM, Vlasova VV, Batina NA, Elgina SI, Mozes VG, Mozes KB, Rudaeva EV
Kuzbass Regional Clinical Hospital named after SV Belyaev, Kemerovo State Medical University, Kemerovo, Russia
GESTATIONAL GIGANTOMASTIA (CLINICAL CASE)
Gigantomastia (macromastia, hypermastia) is a rare disease associated with excessive hypertrophy of the connective tissue of the breast in women. Gestational gigantomastia is a type of disease, the most common type. It develops during pregnancy under the influence of hormonal surges of progesterone, prolactin, and estradiol. More often, gigantomastia is bilateral, less often-unilateral. The disease occurs in one case per 28000-100000 pregnancies. As a rule, the condition develops in the first trimester under the influence of placental hormones. The consequences of the disease are more often observed in women with multiple pregnancies. Approximately 150 cases of gestational gigantomastia have been reported. After childbirth, in some cases, the breasts return to their postpartum state, but with subsequent pregnancy they increase again, usually more significantly. The condition threatens the health of the mother, but has a good outcome for the fetus. Despite the benign nature of gigantomastia, it can cause a dangerous condition and even death from severe infection and cardiopulmonary failure. This article describes a rare clinical case of gestational gigantomastia. Taking into account the optimal chosen management tactics of the patient, a relatively favorable outcome of pregnancy and childbirth for the mother and fetus was obtained.
Key words
: gestational gigantomastia; pregnancy; childbirth
Gigantomastia (macromastia, hypermastia) is a rare disease associated with excessive hypertrophy of the connective tissue of the mammary gland in women [1, 2]. Gestational gigantomastia is a type of disease and the most common type. It develops during pregnancy under the influence of hormonal surges of progesterone, prolactin, and estradiol. The remaining types (juvenile, drug-induced and idiopathic) are less common. More often, gigantomastia is bilateral, less often – unilateral [1, 2]. The largest recorded mass of excised breast tissue was 27.5 kg per breast. Gestational gigantomastia was first described in 1648. The disease occurs in one case in 28,000-100,000 pregnancies. As a rule, the condition develops in the first trimester under the influence of placental hormones. The consequences of the disease are more often observed in women with multiple pregnancies [1, 2]. Approximately 150 cases of gestational gigantomastia have been reported. After childbirth, in some cases, the breasts return to their postpartum state, but with subsequent pregnancy they increase again, usually more significantly. The condition threatens the health of the mother, but has a good outcome for the fetus. Despite the benign nature of gigantomastia, it can cause a dangerous condition and even death from severe infection and cardiopulmonary failure [1, 2]. The factors controlling breast growth are complex and not fully understood, although the role of hormonal influences has been studied and the pathogenesis appears to be related to excessive production of estrogen and prolactin. Imbalance of hormones leads to the development of large and painful breasts. This condition is called gestational gigantomastia - breast hyperplasia during pregnancy. Several cases of gigantomastia have been reported in the presence of normal hormone levels. Consequently, another hypothesis is also true: increased sensitivity of receptors to hormones leads to gigantomastia [1, 2]. Growth hormone and steroids are also known to play a role in the development of the disease. But this reason is still under study. Gestational, or pregnancy-induced, is a rare, benign condition. Characterized by uniform extreme hypertrophy of one or both mammary glands during pregnancy. The etiology and pathogenesis have not been fully established. The disease is believed to be caused by placental hormones. This hypothesis is supported by the fact that excessive increase in breast size is most often observed during the first trimester, when the greatest amount of gonadotropin is produced. The main influence is exerted by prolactin, as well as other hormones: progesterone, estrogen, thyroxine, growth hormone, cortisol, insulin and human placental lactogen [1, 2]. Patients with gigantomastia experience social and psychological problems, as well as difficulties with movement and breathing, including the development of respiratory and heart failure. Due to the large mass of the mammary glands, it is difficult for a woman to breathe, especially when lying on her back. The result is a lack of oxygen. Oxygen deficiency in severe cases leads to hypoxia of all organs, including the cardiovascular system [1, 2]. Massive breast enlargement may be accompanied by thinning of the skin, tissue necrosis, infection and hemorrhage. Emotional, social and psychological problems arise - depression and low self-esteem [1, 2]. In 2010-2013 A study was conducted to study breast tissue samples from patients with macromastia. Samples were obtained by reduction mammoplasty. A total of 198 patients were examined; samples of mammary gland tissue were stained and examined under a microscope. Based on the results of microscopic observation, it was revealed: - normal tissue was present in 98 cases (49.5%), in the rest there was an increased fat content; — in 47.5% of cases a benign fibrocystic change was observed; — in two cases (1%) intraductal papilloma was detected; - in four cases (2%) - malignant formations, including two cases (1%) with invasive ductal cancer (ages 22 and 31 years) and two cases (1%) with lobular carcinoma - precancerous lesions of the lobules of the mammary gland (age 21 and 35 years old); — taking into account intraductal papilloma as a precancerous condition, the overall incidence of malignant tumors reached 3% [1, 2].
Thus, macromastia can be considered a risk factor for malignant neoplasms of the mammary gland. For this reason, it is extremely important to perform histopathological examination after breast reduction or removal surgery [1, 2]. Diagnosis includes examination, history taking, laboratory and instrumental methods. Medical examination and history taking
consist of determining: - breast size; - height, weight and body mass index; - presence of deformation of the chest wall or mammary glands; — dates of the first menstruation and the beginning of breast growth; - medications that the woman took during her life; - family history of breast diseases - hypertrophy and cancer; - pregnancy.
Laboratory diagnostics
includes: - a complete hematological and biochemical study, including determination of calcium levels and levels of thyroid and parathyroid hormones to exclude or correct autoimmune diseases; — determination of the level of prolactin, progesterone and estrogen; — screening of antinuclear antibodies (ANA) to detect autoimmune diseases.
Instrumental diagnostics:
— Ultrasound of the mammary glands. Imaging with ultrasound or mammography may be difficult or technically impossible. In cases where the study can be performed, diffuse hypoechoic (with lower density than neighboring tissues) areas with increased blood supply are determined [3]. — Histological examination reveals significant lobar hypertrophy, proliferation of ducts and periductal fibrosis - the formation of collagen fibers around the milk ducts. In addition, gestational gigantomastia may be accompanied by extensive lobular hyperplasia, dilated milk ducts and pseudoangiomatous hyperplasia - proliferation of breast tissue [3]. Immunohistochemical staining results for estrogen and progesterone receptor expression were positive in more than 50% of epithelial cells [4, 5].
Treatment of gigantomastia can be conservative or surgical. Once the suspected causative factor, such as pregnancy, stops, the breasts may shrink on their own. During this period, it is important to use comfortable, supportive bras. However, significant hypertrophy (more than 0.6-2 kg) does not regress. If there are infections and ulcerations, antibiotics and dressings are prescribed. Drug treatment for hyperprolactinemia includes the use of the dopamine receptor agonist bromocriptine or the less toxic cabergoline. The drugs stop the growth of the mammary glands, but do not reduce breast size. The results of treatment with bromocriptine are contradictory; the doctor can offer such therapy only after assessing all the risks. If bromocriptine is taken during pregnancy, fetal growth should be closely monitored due to the risk of intrauterine growth retardation [6, 7]. Surgical treatment is the main method for gigantomastia.
Preoperative counseling includes: - a thorough discussion of the long-term results of breast reduction, including possible reoperation after pregnancy or if weight changes; — violation or impossibility of breastfeeding after surgery [5].
It is advisable to postpone the operation until the pregnancy is completed or until the fetus reaches viability. Breast size before surgery should be the same for 6-12 months. This will help achieve optimal results [8, 9]. Treatment options include reduction mammoplasty or mastectomy with or without reconstruction.
Reduction mammoplasty is recommended as the first line of treatment for macromastia. The surgery successfully reduces breasts and helps eliminate skin damage and infections associated with breast enlargement. Mastectomy is a surgical operation to remove the mammary gland, performed for relapses after reduction mammoplasty. Mastectomy is necessary for life-threatening complications of gigantomastia, such as infection, hemorrhage, heart failure, massive bleeding, ulceration or necrosis of the breast [10, 11]. Gestational gigantomastia can begin with any pregnancy and recur during subsequent ones. It is extremely important to educate patients about the risks of relapse, especially during further pregnancy. In case of massive gigantomastia, a free nipple transplant may be required, but this leads to lactation disruption. The patient should be carefully informed about this [12, 13]. Hyperprolactinemia (increased prolactin levels) is a common condition in patients with gestational gigantomastia. The best treatment option is a total mastectomy. Possible complications during surgery include severe anemia and bleeding. Mastectomy with implant reconstruction is the preferred treatment method. However, breast prostheses and implants can lead to complications. Measures to prevent gigantomastia include preventing obesity - proper nutrition and exercise, as well as monitoring hormonal levels and taking hormonal medications only as prescribed by a doctor. For women planning a pregnancy, a total mastectomy may be recommended, since the risk of recurrence after reduction mammoplasty is high [14-16]. Considering all of the above, the rare case of gigantomastia in the patient is of practical interest.
Patient L.
For 32 years she was in the Regional Perinatal Center of the Kuzbass Regional Clinical Hospital named after. S.V. Belyaeva with the diagnosis “Pregnancy 26 weeks. Gigantomastia. Lymphovenous insufficiency. Trophic skin ulcer. Chronic feto-placental insufficiency. Chronic fetal hypoxia. Gestational diabetes mellitus. Mild gestational anemia." Upon admission, she complained of significant enlargement of the mammary glands from the first trimester of pregnancy. Observation of a pregnant woman in the antenatal clinic in accordance with Order 572-n of the Ministry of Health of Russia dated November 12, 2012 “On approval of the Procedure for the provision of medical care in the field of obstetrics and gynecology (except for the use of assisted reproductive technologies).” This is the fourth pregnancy, desired, without preconception preparation. The first ended in urgent birth in 2021, fetal asphyxia during childbirth, the son is 3700 g, has delayed speech development, and has had diabetes since the age of 9. The second – in 2021, a failed miscarriage at 4 weeks of pregnancy, with curettage of the uterine cavity. The third in 2021 was a spontaneous miscarriage at 5 weeks of pregnancy. Menstrual function - menstruation from the age of 14, painful, heavy, every 35-45 days, 7 days each. Sexual life from the age of 17. Contraception - COC, while taking it, she noted an enlargement of the mammary glands, and therefore in 2015 she stopped taking COCs. Also, the mammary glands increased in 2021 and 2021 during pregnancies, without returning to their original size. Gynecological diseases: menstrual irregularities, hemorrhagic form of ovarian apoplexy (laparotomy, ovarian resection in 2013), unspecified secondary infertility, endometrial polyp (hysteroresectoscopy in 2021), after which dydrogesterone was prescribed, which also resulted in enlargement of the mammary glands . In 2015, 2021, 2021 and 2021 removal of fibroadenomas of the mammary glands on both sides. STIs were examined and found to be absent. Denies injuries. Denies bad habits. Somatically – since 2010, autoimmune thyroiditis, hypothyroidism, receiving L-thyroxine 25 mcg, chronic pyelonephritis, cystitis, varicose veins of the lower extremities since adolescence. Allergological history - cannot tolerate trichopolum, nasal congestion. Heredity is aggravated on the mother's side, breast cancer in an aunt (mother's sister).
Course of pregnancy:
At 3-4 weeks of pregnancy, I was bothered by nagging pain in the lower abdomen; at 4-5 weeks, there was blood discharge from the genital tract; inpatient treatment was performed (dydrogesterone according to the scheme of threatened miscarriage, followed by taking 10 mg 3 times a day until 20 weeks of pregnancy). From 3 weeks of pregnancy she notices an enlargement of the mammary glands. Consulted at the KOOD - an ultrasound of the mammary glands was performed, evidence of the presence of hyperplasia of mammary gland tissue, focal neoplasms in both mammary glands. A diagnosis of Gigantomastia, Edematous-infiltrative form was made? S-sr mammary glands? Observation and follow-up examination in a month are recommended. From 20 weeks of pregnancy, treatment by a surgeon for trophic erosions of the mammary glands. At 21 weeks of pregnancy there was bleeding from a varicose vein in the right breast; hemostatic sutures were applied. At 22 weeks of pregnancy - a consultation with a mammologist at the Regional Perinatal Center, an ultrasound examination of the mammary glands was repeated - gigantomastia, lymphostasis, giant fibroadenomas on the right, swelling and infiltration of the mammary glands, lymphadenopathy. Diagnosis: “Gigantomastia of both mammary glands, secondary lymphostasis. Trophic erosion of both mammary glands. Fistulas of postoperative scars after previously removed fibroadenomas. Fibroadenoma of the right breast." Treatment by a local surgeon and ultrasound monitoring every month are recommended. Consulted by an endocrinologist at 22 weeks of pregnancy - “Gestational diabetes mellitus, compensated by diet.” At 26 weeks of pregnancy, there was a threat of premature birth, she was in the obstetric department of pregnant women at the place of residence, tocolysis was performed with ginipral, prevention of fetal respiratory distress syndrome with dexamethasone at a dose of 24 mg, and for further treatment she was transferred to the Regional Perinatal Center. Upon admission, external and internal obstetric examination was unchanged. The mammary glands are extremely enlarged, edematous, cyanotic in color, varicose veins and collateral networks are prominent. The nipples are retracted, the areolas are stretched. On the right on the lateral surface there is a skin defect up to 8 cm in diameter with necrotic masses, nearby there are 2 defects up to 2 cm and 1 cm. On the left on the lateral surface there are skin defects with signs of granulation and epithelization up to 3, 1, and 0.8 cm (photo 1 , 2, 3).
Photo 1. Patient L. View of the patient’s mammary glands upon admission to the Kuzbass Regional Clinical Hospital named after. S.V. Belyaev Photo 1. Patient L. View of the patient's mammary glands upon admission to the Kuzbass Regional Clinical Hospital named after SV Belyaev
Photo 2. Patient L. View of the patient’s mammary glands upon admission to the Kuzbass Regional Clinical Hospital named after. S.V. Belyaev Photo 2. Patient L. View of the patient's mammary gland upon admission to the Kuzbass Regional Clinical Hospital named after SV Belyaev
Photo 3. Patient L. View of the patient’s mammary glands upon admission to the Kuzbass Regional Clinical Hospital named after. S.V. Belyaev Photo 3. Patient L. View of the patient's mammary gland upon admission to the Kuzbass Regional Clinical Hospital named after SV Belyaev
An examination was carried out at the Regional Perinatal Center. Ultrasound of the uterus and fetus - pregnancy 26 weeks and 4 days, echo signs of feto-placental insufficiency, diffuse changes in the placenta. Doppler examination revealed no disturbance of uteroplacental blood flow. According to ultrasound of the mammary glands, in the structure of the right mammary gland there is a fibroadenoma measuring 28-45 cm. In the structure of both mammary glands, there are numerous small cysts up to 5 mm. On the right, a fistulous tract of up to 41 mm is identified with parietal hyperechoic inclusions of heterogeneous contents. On the left there are two fistula tracts - one 24 mm, the other 23 mm. In the axillary areas, the lymph nodes are enlarged to 24 mm, anechoic, and deformed. The woman is examined by a surgeon. Secondary surgical treatment and necrectomy of the wound were performed. The blood prolactin content was 3081.5 nmol/l, estradiol 10,000 pg/ml. Positive C-reactive protein result, negative over time. Hemoglodin level – 91 g/l. Culture of discharge from the wound - Staphylococcus aureus 107, sensitive to cefoxitin, ceftriaxone, gentamicin, erythromycin, vancomycin, was cultured. Four times normoglycemia. A study of biopsy material from a wound of the mammary glands showed adenosis, with foci of necrosis, serous-purulent inflammation, with extensive marginal necrosis with hemorrhages. Antibacterial (ceftriaxone 2 g IV), antianemic (Ferrum-lek 100 mg 2 times a day) therapy was carried out, correction of hypothyroidism was continued (L-thyroxine 25 mcg per day), upon receipt of the results of a hormonal examination, Dostinex 0 was added to treatment .5 mg for 3 days. Taking into account the extreme rarity of the pathology, a telemedicine consultation was carried out with the Federal State Budgetary Institution National Medical Research Center of AGP named after. IN AND. Kulakov to decide on a mastectomy. During the consultation, the tactics of the doctors of the Regional Perinatal Center were recognized as correct, and the mastectomy was planned at the federal center. The patient consented to surgical treatment and hospitalization. Taking into account the anemia and the upcoming radical surgery, the treatment of anemia was replaced with intravenous drugs. The patient was hospitalized by air to the Federal State Budgetary Institution National Medical Research Center of AGP named after. IN AND. Kulakov, accompanied by an anesthesiologist. Immediately after transporting the woman to the Federal State Budgetary Institution National Medical Research Center for AGP named after. IN AND. Kulakova, at 28 weeks of pregnancy, underwent a bilateral mastectomy, the patient was discharged on the 10th day after the operation in satisfactory condition (photo 4, 5).
Photo 4. Patient L. View of the patient's mammary gland after surgery
Photo 5. Patient L. View of the patient's mammary gland after surgery
Pregnancy monitoring continued at the place of residence and at the Regional Perinatal Center. At 38 weeks of pregnancy, the woman was admitted for delivery to the Regional Perinatal Center, where, at 38 weeks of pregnancy and 6 days, an emergency surgical delivery was performed due to primary incoordination of labor. A daughter was born, weighing 3160 g, height 52 cm, Apgar score 8/9 points. The late postpartum postoperative period was complicated by decidual endometritis, for which the woman was transferred to the gynecological department, where she underwent antibiotic therapy, two sanitary hysteroscopies, and manual vacuum aspiration of the uterine cavity. The woman was discharged from the department on the 24th day of the postpartum period in satisfactory condition.
CONCLUSION
This article describes a rare clinical case of gestational gigantomastia. Taking into account the optimal chosen tactics for managing the patient, a relatively favorable outcome for the woman, pregnancy and childbirth for the mother and fetus was obtained.
Funding and conflict of interest information
The study had no sponsorship. The authors declare that there are no obvious or potential conflicts of interest related to the publication of this article.
LITERATURE / REFERENCES:
1. Rutherford CL, Hsieh MKH, Tan HM, Twoon M, Kong TY. A Rare Case of Persistent Unilateral Gestational Gigantomastia. Plast Reconstr Surg Glob Open.
2019;
7(8): e2372. DOI: 10.1097/GOX. 0000000000002372 2. Das L, Rai A, Vaiphei K, Garg A, Mohsina S, Bhansali A, et al. Idiopathic gigantomastia: newer mechanistic insights implicating the paracrine milieu. Endocrine.
2019;
66(2): 166-177. DOI: 10.1007/s12020-019-02065-x 3. Türkan H, Gökgöz MŞ, Taşdelen İ, Dündar HZ. Gestational Gigantomastia. J Breast Health.
2016;
12(2): 86-87. DOI: 10.5152/tjbh. 2021.2852 4. Cho MJ, Yang JH, Choi HG, Kim WS, Yu YB, Park KS. An idiopathic gigantomastia. Ann Surg Treat Res. 2015; 88(3): 166-169. DOI: 10.4174/astr. 2015.88.3.166 5. Wolfswinkel EM, Lemaine V, Weathers WM, Chike-Obi CJ, Xue AS, Heller L. Hyperplastic Breast Anomalies in the Female Adolescent Breast. Semin Plast Surg.
2013;
27(1): 49-55. DOI: 10.1055/s-0033-1347167 6. Debra Rose Wilson. What is Gigantomastia? //healthline.com. 2017; 8 7. Rabail Raza, Kulsoom Fatima. Gigantomastia: A case report with review of literature. Open Journal of Clinical & Medical Case Reports.
2017;
3 8. Swelstad MR, Swelstad BB, Rao VK, Gutowski KA. Management of gestational gigantomastia. Plast Reconstr Surg.
2006;
118(4): 840-848 9. Fatma Dilek Dellal, Didem Ozdemir, Cevdet Aydin, Gulfem Kaya, Reyhan Ersoy, and Bekir Cakir. Gigantomastia and Macroprolactinemia Responding to Cabergoline Treatment: A Case Report and Minireview of the Literature. Case Reports in Endocrinology
.
2016; 2:1-5. DOI: 10.1155/2016/3576024 10. Ji Hyeon Cha, Hak Hee Kim, Sun Mi Kim, Myung Hee Seo, Hoi Soo Yoon. Breast Gigantism Induced by D-Penicillamine: Case Report. J Korean Radiol Soc.
2004;
50: 213-215 11. Elgina SI, Ushkova GA, Niklina EN. Reproductive system of full-term and premature newborn girls. Fundamental and clinical medicine .
2016;
1(3): 39-45. Russian (Elgina S.I., Ushakova G.A., Nikulina E.N. Reproductive system of full-term and premature newborn girls // Fundamental and Clinical Medicine. 2021. No. 1(3). P. 39-45) 12. Nikolaeva LB, Ushakova GA, Elgina SI. Forecast of population reproduction and reproductive health of girls of Kuzbass. Mother and Baby in Kuzbass.
2010;
1(40: 19-27. Russian (Nikolaeva L.B., Ushakova G.A., Elgina S.I. Forecast of population reproduction and reproductive health of girls in Kuzbass //Mother and Child in Kuzbass. 2010. No. 1(40) . pp. 19-27) 13. Elgina S.I. Clinical assessment of the reproductive system of newborn girls and prediction of violations of its formation. Reproductive health of children and adolescents .
2009; 1: 43-47. Russian (Elgina S.I. Clinical assessment of the reproductive system of newborn girls and prediction of disorders in its development // Reproductive health of children and adolescents. 2009. No. 1. P. 43-47) 14. Apykhtina NA, Elgina SI. Reproductive health of adolescent girls in the Kemerovo region.
Reproductive health of children and adolescents.
2016; 2: 30-31. Russian (Apykhtina N.A., Elgina S.I. Reproductive health of teenage girls in the Kemerovo region //Reproductive health of children and adolescents. 2021. No. 2. P. 30 -31) 15. Talghini S. Is macromastia a risk factor for breast cancer? A study on 198 patients.
Pak J Biol Sci.
2013;16(21): 1348-1352 16. Ezem BU, Osuagwu SS, Opara KA.
Gestational gigantomastia with complete resolution in a Nigerian woman. BMJ Case Rep.
2011; 2011: bcr0120102632. DOI: 10.1136/bcr.01.2010.2632
Address correspondence to:
ELGINA Svetlana Ivanovna 650029, Kemerovo, st. Voroshilova, 22 a, Federal State Budgetary Educational Institution of Higher Education Kemerovo State Medical University of the Ministry of Health of Russia Tel.; Email: [email protected]
Information about authors:
SHIBELGUT Nona Markovna Ph.D. honey. Sciences, Deputy Chief physician for obstetric care, State Autonomous Institution KOKB named after. S.V. Belyaeva, Kemerovo, Russia E-mail: [email protected]
VLASOVA Veronika Valerievna Ph.D. honey. Sciences, Deputy Chief Physician for Gynecological Care, State Autonomous Clinical Hospital named after. S.V. Belyaeva, Kemerovo, Russia E-mail: [email protected]
BATINA Natalya Anatolyevna Head. maternity department, GAUZ KOKB named after. S.V. Belyaeva, Kemerovo, Russia E-mail: [email protected]
ELGINA Svetlana Ivanovna Doctor of Medicine. Sciences, Associate Professor, Professor of the Department of Obstetrics and Gynecology named after. prof. G.A. Ushakova, Kemerovo State Medical University, Ministry of Health of Russia, Kemerovo, Russia E-mail: [email protected]
MOSES Vadim Gelievich Doctor of Medicine. Sciences, Associate Professor, Professor of the Department of Obstetrics and Gynecology named after. prof. G.A. Ushakova, Kemerovo State Medical University, Ministry of Health of Russia, Kemerovo, Russia E-mail: [email protected]
MOSES Kira Borisovna Assistant, Department of Polyclinic Therapy and Nursing, Kemerovo State Medical University of the Ministry of Health of Russia, Kemerovo, Russia
RUDAEVA Elena Vladimirovna Ph.D. honey. Sciences, Associate Professor, Associate Professor of the Department of Obstetrics and Gynecology named after. prof. G.A. Ushakova, Kemerovo State Medical University, Ministry of Health of Russia, Kemerovo, Russia E-mail: [email protected]
Information about authors:
SHIBELGUT Nona Markovna candidate of medical sciences, deputy chief physician for obstetric care, Kuzbass Regional Clinical Hospital named after SV Belyaev, Kemerovo, Russia E-mail: [email protected]
VLASOVA Veronika Valerievna candidate of medical sciences, deputy chief physician for gynecological care, Kuzbass Regional Clinical Hospital named after SV Belyaev, Kemerovo, Russia E-mail: [email protected]
BATINA Natalya Anatolyevna head of the maternity department, Kuzbass Regional Clinical Hospital named after SV Belyaev, Kemerovo, Russia E-mail: [email protected]
ELGINA Svetlana Ivanovna doctor of medical sciences, docent, professor of the department of obstetrics and gynecology named after prof. GA Ushakova, Kemerovo State Medical University, Kemerovo, Russia E-mail: [email protected]
MOZES Vadim Gelievich doctor of medical sciences, docent, professor of the department of obstetrics and gynecology named after prof. GA Ushakova, Kemerovo State Medical University, Kemerovo, Russia E-mail: [email protected]
MOZES Kira Borisovna assistant, department of polyclinic therapy and nursing, Kemerovo State Medical University, Kemerovo, Russia
RUDAEVA Elena Vladimirovna candidate of medical sciences, docent, docent of the department of obstetrics and gynecology named after prof. GA Ushakova, Kemerovo State Medical University, Kemerovo, Russia E-mail: [email protected]
View statistics
Loading metrics...
Links
- There are currently no links.