BRCA - what is it and how is it related to breast cancer
This four-letter acronym has received a lot of attention, although most people don't know what it stands for, what it does, or whether it applies to them.
BRCA are two genes that we all have: BRCA-1 and BRCA-2 (the acronym stands for BReast CAncer). Healthy BRCA genes suppress the growth of tumor cells by repairing or destroying damaged cells before they form a mass.
But in some families, the BRCA genes are damaged and passed on from generation to generation. Less than 10% of all breast cancers and 14% of ovarian cancers are caused by the BRCA gene or another genetic mutation inherited from either parent.
Yes, in order to accurately find out about your genetic mutations and possible dangers, you need to know the history of your father’s family. You got half of your DNA from him, and half of all BRCA mutation carriers are male.
In the general population, BRCA mutations occur in approximately one in 450 people, but in Ashkenazi Jews (the Jewish population of Germany, Poland, Lithuania, Ukraine and Russia - in contrast to Sephardic Jews, who originate mainly from Spain, France, Italy and North Africa) is carried by every 40th person. Given these numbers, Ashkenazi Jewish women who have a family history of breast or ovarian cancer should take a genetic test (more on this below).
Why are mutations of the BRCA-1 and BRCA-2 genes dangerous?
Why is BRCA so important?
If you are a carrier of this mutation, your risk of breast cancer is 25 times higher than the average 50-year-old woman, and your risk of ovarian cancer is 30 times higher than the average 50-year-old woman. Women who are BRCA-1 carriers are 87% more likely to develop the disease during their lifetime, and 54% more likely to develop ovarian cancer during their lifetime. I worry a little more about the breasts of my patients with BRCA-1, because 70% of the cancers they develop are more aggressive, which almost always require chemotherapy even at the first stage.
Because the BRCA genes spell trouble for both breasts, once you get cancer, you have a 40% to 65% chance of developing cancer in the other breast as well. As you can imagine, with this level of risk, many BRCA carriers who have cancer in one breast choose to have a double mastectomy.
Since the average age of diagnosis for cancers with a BRCA-1 mutation is 44 years and those with a BRCA-2 mutation is 47 years, the sooner you learn about this gene, the better you can take preventive measures.
And breasts and ovaries aren't everything: BRCA patients also need to be screened for pancreatic cancer (2-5% chance), and BRCA-2 carriers need to be wary of melanoma (2-5%). By comparison, without a BRCA gene mutation, the risk of breast cancer is 12.4%, ovarian cancer is 1.4%, pancreatic cancer is less than 1%, and melanoma is 2%.
Men with BRCA are also at risk. Male breast cancer is more common in BRCA-2 carriers than in BRCA-1 carriers (8% vs. 1.8%). In addition, BRCA-2 increases the risk of prostate cancer much more than BRCA-1 (16–25% and minimal increase, respectively).
Like women, BRCA-positive individuals may develop pancreatic cancer (3–6%), and BRCA-2 carriers require screening for melanoma (2–6%). In men without a BRCA gene mutation, the risk of breast cancer is 0.001%, prostate cancer - 14%, pancreatic cancer - 1.1%, and melanoma - 2.5%.
Which breast is bigger?
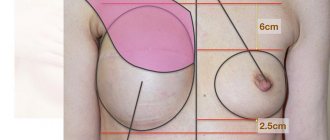
3. The left breast is slightly larger than the right
Experts are confident that finding absolutely identical breasts is very difficult. It is very rare that both breasts are exactly the same size. As a rule, the right breast is slightly smaller than the left in size.
Most often the difference is little noticeable. But nevertheless, it exists. Nipples may also differ from each other in radius of circumference.
4. The first thing men pay attention to is their breasts.
Research conducted at a University in Wellington has proven that a woman's bust is the first thing that members of the opposite sex look at. In addition, looking at breasts takes more time than looking at other parts of the body.
A new theory about why men love women's breasts
However, psychologists do not see anything wrong with this. On the contrary, experts recommend that men look at women's breasts as often as possible. In their opinion, this practice can improve health and add 4-5 years to life.
5. Men can also breastfeed
This doesn't happen often, but men do have the potential to produce milk. In rare cases of hormonal imbalance,
especially after treatment of cancer, a man’s breasts are able to produce milk similar to that which a woman feeds her offspring.
6. The country with the most busty women is England
Research carried out by the famous lingerie manufacturer Triumph has shown that British women are the most busty in all of Europe. More than half of the residents of Foggy Albion wear size 4.
Denmark is in second place, followed by Holland. It is in these countries, according to experts, that women have an impressive bust size. Women with the smallest breasts live in Italy. More than 68 percent of Italian women wear size 2.
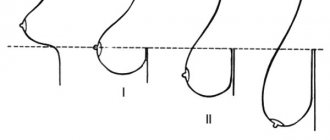
7. On average, female breasts weigh about 0.5 kg
Typically, each breast contains about 4-5 percent of total body fat and makes up about 1 percent of a woman's body weight.
Should you get tested for BRCA: 7 pros, 1 con
Patients often tell me, “I don’t want to know if I have the mutation. What will it change?" In fact - a lot of things!
Firstly, there is a high probability that you do not have any mutation, and knowing this will make you much less worried.
Second, if you test positive for the mutation, you will be given more intensive surveillance (such as a breast MRI), and the extra vigilance may have benefits, such as helping to detect cancer early with better images.
Third, your doctors may want to test you for other cancers related to your mutation.
Fourth, your breast surgeons can offer you effective medications and surgeries to reduce your risk of developing the disease.
Fifthly, it will also be useful for other family members to know about your status.
Sixthly, you will have additional motivation to do something with controlled risks - the same diet and weight, and this will be good for your health in any case.
And finally, if you are planning to start a family, then you will have the opportunity not to pass this mutation on to inheritance.
On the other hand, if knowing about the mutation will only increase your anxiety and you will refuse any intervention, then perhaps it really is better not to know.
Plastic breast augmentation
11. Breast augmentation is the most common plastic surgery in the United States.
More than two million American women have artificial breasts. Breast implants have overtaken rhinoplasty and liposuction in popularity. The average age when a woman decides to have breast augmentation is 34 years.
12. In China, you can specialize in Breast Science.
In Hong Kong, anyone can obtain an advanced degree in Breast Science if they wish. The Hong Kong Polytechnic University will teach students how to properly design and sew a bra.
It is worth noting that the most diligent and diligent students have very good success in this matter: the work of some of them was presented at one of the exhibitions of intimate clothing in China.
Who should consider genetic testing: 9 red flags
Given the high likelihood of cancer of the breast, ovaries or other organs due to various mutations, the first “red flag” that warns you about the need for genetic testing is cases of cancer among relatives of both sexes.
To do this, you will need to do some research. Find information about your first, second and third generation relatives on your mother's and father's sides. Do you know why your dad's brother died? (I don’t even know if my dad had a brother.) Who had what type of cancer?
If you have any of the nine red flags (or more than one relative on the same side of the family tree has them), your risk of a genetic mutation is greater than 10% and you should consider genetic testing. These are the “red flags”:
- Breast cancer before age 50 or ovarian cancer at any age in two female relatives.
- Ashkenazi Jewish descent plus one breast cancer before age 50 or ovarian cancer at any age.
- Breast cancer in any male relative.
- A known carrier of the BRCA gene mutation in the family (if in close relatives, then the probability of transmission of the carrier is 50%).
- You yourself have breast cancer before the age of 50.
- You have two types of breast cancer (not recurrence) at any age.
- Triple negative breast cancer before age 60.
- Ashkenazi Jewish descent and breast cancer at any age.
- History of cancer: two or more family members on one side: breast, ovarian, pancreatic, prostate, uterine, colon, stomach and/or melanoma.
Saliva or blood are usually donated for analysis; You can either test for the presence of the entire spectrum of genes that cause cancer, or only specific genes that interest you. A geneticist will discuss the implications of testing with you and help you understand how the presence or absence of a genetic mutation affects your risk of cancer and options for reducing it.
You have been found to have a mutation in the BRCA-1 and BRCA-2 genes: what next?
If doctors tell you that you have a genetic mutation, you will have a whole arsenal of new weapons. Take Sarah, a newly engaged 26-year-old second-grade teacher, as an example. She has a BRCA-1 gene mutation, her mother died of ovarian cancer at 44 (Sarah was fourteen at the time), and her maternal aunt died of breast cancer at 51.
Sarah had already visited several doctors, but only became more confused. I quickly learned that Sarah had wanted to have two children and breastfeed them for as long as she could remember. She loves her breasts very much, but believes that after her destiny to feed children is fulfilled, she will worry too much to keep them.
Along with her supportive fiancé Doug, we looked at Sarah's real-life risks of breast and ovarian cancer, broken down by decade over the next 65 years (because I expect her to live into her nineties). With this new information, she no longer considered the situation urgent and was able to think more calmly.
We developed a strategy that they both found acceptable, which included breast exams and regular imaging. They decided to immediately plan the pregnancy and remove the ovaries after the children were born. Sarah planned a bilateral prophylactic mastectomy at age 35. Sarah and Doug left the office armed with a proactive plan that suited their situation.
If you are a carrier of a genetic mutation and I am meeting you for the first time, I will try to learn as much as possible about your prejudices and personality. answer the following questions for yourself :
- How have other people's experiences with cancer affected your perception of treatment and side effects?
- Are you in a long-term relationship, married or living alone?
- Have you given birth? Do you want to have children? Is breastfeeding a priority for you?
- What do breasts mean to you in terms of appearance, sexual pleasure and femininity?
- Can you live with peace of mind knowing about the risk, or does it rob you of peace? Which at-risk organ are you more concerned about, the breasts or the ovaries, and why?
- What is your profession and will the plans we are making interfere with your work or travel?
The answers to these questions and other information specific to you will help the doctor and even you in this process of self-discovery.
Advertising
Angelina Jolie and facial plastic surgery
Angelina Jolie's lips, nose and cheekbones have long become symbols of female attractiveness and sexuality, and therefore, to the delight of plastic surgeons, millions of women want to have exactly the same ones. Among those who have already “acquired” Jolie’s lips, for example, are American actress Megan Fox and Russian “Cinderella” Victoria Bonya. The star has many imitators and doubles, which means she rightfully takes her place among the most beautiful and desirable women on the planet. The perfect image of the actress gives rise to a lot of rumors, including those questioning the naturalness of her beauty; it is possible that she had the following done:
Rhinoplasty. Angelina Jolie made a name for herself in the late 90s by starring in the film “Hackers.” Around this time, changes occurred in her appearance - the actress corrected the shape of her nose, including narrowing the back. This plastic surgery added sophistication to Jolie’s face, and she was literally showered with offers from directors who saw her in the role of a bold and courageous, but at the same time sexy heroine. Rhinoplasty is obvious if you compare the photos of Jolie before and after the operation. So, at the age of 16, Angelina had a snub nose and quite wide, and a few years later it became “Greek” - surprisingly smooth and graceful. The operation was done successfully - the face did not lose its individuality, which allows the actress to deny plastic surgery, but the shape of the nose clearly changed, and this could not have happened by itself.
Correction of cheeks and cheekbones. In her youth, Angelina had plump cheeks and smoothed cheekbones, but now the opposite is true - her cheeks are slightly sunken, and her cheekbones have gained volume, making the actress look at least ten years younger. It’s not difficult to calculate how old Angelina Jolie is - she was born in 1975, which means she celebrated her 41st birthday in 2021. It’s possible that fillers, such as high-density Radiesse, help maintain the relief of the star’s cheekbones, or she underwent lipofilling, a plastic surgery to transplant her own fatty tissue into the cheekbone area. Many admirers of the actress’s talent do not agree with the version of cheekbone plastic surgery; they believe that the cheekbones and cheeks have changed shape due to the star’s weight loss, and in addition, a similar effect can be easily achieved by directing light onto the face in a certain way. As evidence, the film Maleficent is cited, where Jolie emphasized her cheekbones with the help of professional makeup.
Facelift . In 2009, photos appeared that suggested that Angelina Jolie had undergone a surgical facelift. According to some experts, the scar behind the ear, resembling a cut mark, could have remained after otoplasty (ear plastic surgery) or after a facelift. Others, for example, Jennifer Walden (American plastic surgeon), believes that after the mentioned operations, completely different scars remain: firstly, they try to make incisions in the scalp, and secondly, the skin is incised in a different direction. In addition, there are suggestions that the scar remained after the removal of the birthmark, and a similar effect could have been caused by Botox injections - since some of the muscles are paralyzed, other nearby muscles try to take over their functions. Although, perhaps, the scars behind the ear and on the actress’s neck are a photo montage or a banal mark from the temples of sunglasses.
Lip shape correction. Angelina Jolie is unlikely to have had lip surgery – she naturally has voluminous lips, which is convincingly proven by photos of the actress in childhood and adolescence. Moreover, fans enthusiastically share their observations: looking at photos of the star’s own children, they discovered that they inherited her mouth shape, which means it’s pointless to talk about any plastic surgery. All of the above is true, but you need to make an adjustment for age - after forty, lips usually lose volume and become thinner. To prevent this from happening, you need to maintain their shape with the help of hyaluronic fillers, for example, Princess Volume, which is probably what Angelina Jolie does, whose photos before and after plastic surgery show that she manages to maintain lip volume at a “young” level.
Eye shape correction. It is unlikely that the star would correct her almond-shaped eyes; rather, she adds sexiness to her look with competent makeup.
It's easy to notice that the star quite often uses false eyelashes or extensions.
Prevention of breast cancer: observation or surgery?
Genetic mutations present patients with a choice: observation or surgery. The example of Angelina Jolie, who chose the second option, is widely known. Others do not want to go near a scalpel, preferring to take medications. Still others focus on lifestyle factors such as nutrition, weight loss, exercise, and an in-depth screening regimen.
Increased risk alone does not mean you have to follow any single protocol. I want to help women find a path that allows them to feel calm and confident in their choices.
Remember: surveillance is not prevention, but simply the hope of finding a tumor as early as possible. The route of observation is x-rays and examinations, and possibly risk-reducing medications and traditional Chinese medicine. Here is the surveillance plan I use for women at increased risk:
- At age 18, monthly self-examinations (MSEs) begin and continue until the end of life.
- At the same age of 18, I begin conducting clinical trials (CTs) every six months.
- At age 25, we introduce annual breast MRI with macrocyclic gadolinium and annual ultrasound of the entire breast six months after the MRI.
- At age 30, we also start annual mammograms.
- Men with a BRCA gene mutation are required to undergo self-exams and clinical testing starting at age 35, and prostate screening starting at age 45.
My greatest hope is that a solid monitoring plan will replace anxiety with answers and fear with confidence.
Largest natural breasts
The owner of the largest natural breasts is Norma Stitz.
2. There is an American NGO that fights for the rights of topless women.
Representatives of "Go Topless"
argue that a woman has the same constitutional right and can, on an equal basis with men, appear in public places with bare breasts.
They often speak at various meetings and promote the so-called “topless” for the fairer sex. The main demand of participants in such events is to achieve the lifting of the ban on women appearing in public places with their upper body uncovered.
What can you do to prevent ovarian cancer?
When it comes to ovarian cancer, our complete failure to detect it early is disappointing and worrying. I recommend discussing with your gynecologist whether it is worthwhile to conduct a pelvic examination, vaginal ultrasound, and tests for the tumor marker CA-125.
Oral contraceptives (OCs), also known as birth control, reduce the risk of ovarian cancer by 50% and do not increase the risk of breast cancer significantly enough to negate this protection. All BRCA gene carriers who have ovaries, have not yet reached menopause, and are not trying to conceive should take OCs (unless contraindicated), even if they have breasts. I can watch the breasts, but the ovaries are hidden from view, and when a tumor develops in them, the likelihood of survival is quite small.